The dangers of opiate addiction are well-known. With overdose deaths continuing to rise, the elevated role of dangerous synthetic opioids, such as fentanyl and carfentanil, and the continued abuse of prescription medications, millions of Americans are straddling a line between life and death every day.
Due to the dangers of opioid abuse and the significant consequences to life, love and employment that can accompany drug addiction, many substance users want to get clean. However, this is often easier said than done. Overcoming opioid effects, including the painful process of withdrawal, can be a significant hurdle that isn’t a walk in the park for anyone. If you or someone you love is living with an addiction to heroin or prescription opioids, this is what you need to know about the withdrawal process and how long opiate withdrawal takes.
Physical Opioid Dependency
Opioids, like other easily abused substances, are enjoyed primarily for their side effects. When high on drugs such as heroin, users feel euphoric, carefree and on top of the world. However, addiction goes far beyond the sensations of intoxication.
Opioid use changes the chemistry of the brain, influencing how sensations are processed. When in use, opiates bind to receptors within the brain, reducing sensations of pain and increasing feelings of euphoria. However, over time, the body builds resistance to the effects of opioids, and increased use is required to stimulate the same response.
When opioids aren’t being used, the body is unable to feel pleasure normally due to the effects of high levels of opioids on the receptors throughout the nervous system.
The negative side effects that come from a lack of access to substances are known as withdrawal — and the associated symptoms can be difficult to handle.
Going Cold Turkey
To some drug users, going cold turkey seems like the easiest avenue. It requires no money and can be done at home, so it’s often the preferred method for those quitting for the first time. But while some people can successfully withdraw from opioids by quitting without assistance, most can’t.
For most users, all the determination in the world isn’t enough to stand up to the pain of withdrawal. As soon as the worst of the symptoms develop, many users are willing to do whatever it takes to access additional drugs.
How Long Does Opiate Withdrawal Last?
Depending on the severity of the addiction, opiate withdrawal can last a week or more. Many people are unable to withstand the experience, especially if they’re trying to balance school, work or family at the same time.
Unfortunately, trying to quit and failing can harm an addict’s subsequent attempts to get clean. Once a person knows what to expect from the withdrawal process, they’re much less likely to put themselves through it again. Some opioid users start to believe they’ll never be able to quit, even with medical assistance. This increases the likelihood that their addiction will worsen and that they’ll overdose.
Withdrawal From Opioids
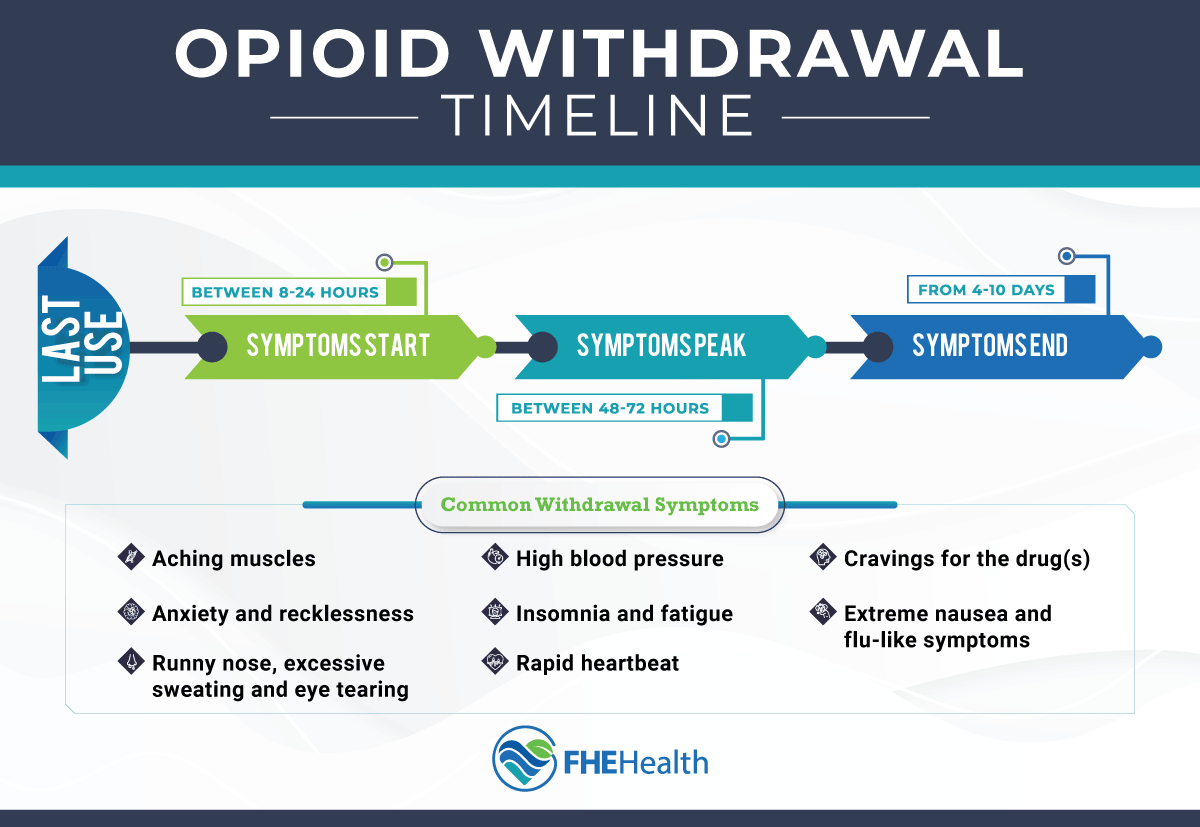
Withdrawing from opioids is extremely unpleasant. With the potential to last for weeks, opioid withdrawal takes physical and mental strength to navigate. Although withdrawal symptoms often vary from one person to the next, the most common symptoms include:
- Aching muscles
- Anxiety and recklessness
- Runny nose, excessive sweating and eye tearing
- Extreme nausea and flu-like symptoms
- Insomnia and fatigue
- Rapid heartbeat
- High blood pressure
When combined with strong cravings for additional drugs, these symptoms are completely debilitating and make it impossible to carry out regular daily activities.
The Stages of Opiate Withdrawal
For most users, opioid withdrawal follows a relatively predictable timeline. The first and second weeks are known as the acute withdrawal stage.
- First 48 Hours
The initial withdrawal symptoms start 6 to 12 hours after the user’s last hit. They include muscle aches, chills, sweating, eye tearing and anxiety. These effects worsen over the next 24 to 48 hours, with nausea and flu-like symptoms developing. During this time, cravings intensify significantly. The user finds it difficult to think about anything else.
During the first stages of opioid withdrawal, it’s virtually impossible to go to school or work or attend family events. Most users can’t do much besides staying in bed or lying on the couch. - 72 to 120 Hours
Days 3 to 5 are often considered the worst. Symptoms usually peak at this point, with gastrointestinal distress, anxiety, sweating and insomnia reaching their peak. Withdrawal symptoms are usually so intense that the patient may not even be able to focus on something as simple as watching TV or reading a book.
At this stage of the withdrawal process, sleeping and keeping food down are challenging. It’s so uncomfortable many people relapse during this time frame. - 120 Hours and Beyond
After 120 hours, the effects of withdrawal begin to subside. Insomnia, flu symptoms and nausea settle enough that the patient may be able to start eating normally again. They still experience cravings, but these aren’t as intense as at the beginning.
Symptoms continue to decrease over the next 3 to 5 days. After 2 weeks, the worst is usually over. - PAWS
An acronym for post-acute withdrawal syndrome, PAWS follows the acute withdrawal phase and describes anything beyond the first 1 to 2 weeks of withdrawal. While the worst symptoms cease after the first 7 to 10 days, PAWS can continue for months or years. Symptoms are wide-ranging and can include mood swings, trouble concentrating and sleeping issues. Everyone experiences PAWS differently, and it often plays a role in relapse.
PAWS episodes can come and go, often lasting several days at a time. Episodes don’t necessarily have any specific triggers. Intermittent symptoms can occur for 2 to 3 years.
Supervised Withdrawal
The challenges of quitting cold turkey without supervision are well-documented. The process is so arduous that most professionals agree that opiate addicts should undergo supervised withdrawal if possible.
This process takes place within a professional opioid treatment center with doctors and nurses. Instead of letting symptoms run their course, addiction medicine specialists provide the patient with medication and therapy to manage their withdrawal symptoms. These include over-the-counter pain medication, sleep aids and drugs to help reduce fever. Medical professionals can also administer a drug called naltrexone to reduce some of the effects opioids have on the body.
Common Prescription Opiates
In the United States, opiates are commonly prescribed by physicians to help treat pain and are known under the following names:
- Hydrocodone (Vicodin®) oxycodone (OxyContin®, Percocet®)
- Oxymorphone (Opana®)
- Morphine (Kadian®, Avinza®)
- Codeine
- Fentanyl
When taken as prescribed over a short period, these medications don’t usually pose a danger to the person taking them, but they carry a high potential for misuse. For instance, people who are prescribed opiates to manage chronic (long-term) pain might find themselves needing more and more of the medication to get the desired effect. This is known as tolerance. Over an extended time, these patients experience withdrawal symptoms when they stop taking their medication, even if they don’t consider themselves addicts per se.
Tapering in a Supervised Setting
In some cases, a medical professional may recommend tapering off opiates instead of quitting cold turkey. Tapering helps reduce a person’s reliance on a drug slowly, which is often safer and more comfortable for the person who’s detoxing.
In a tapering situation, a doctor provides opioids in progressively smaller doses, sometimes daily and sometimes over a longer period, depending on the circumstances. The process is still uncomfortable, but it lets users adapt to smaller and smaller doses gradually. The withdrawal symptoms are much less intense this way, making the detoxing process more bearable and thus improving the patient’s chances of success.
Tapering isn’t necessary for everyone, but it can be a great option for opiate addicts who’ve tried and failed to detox multiple times or who’ve been using opioids for an extended time.
Why Professional Help Matters
In 2020, around 2.7 million Americans over the age of 12 suffered from an opioid use disorder. Attempting to detox from an opiate addiction without professional help is associated with much more severe withdrawal symptoms and a higher relapse rate.
Fortunately, detoxing in the right environment can vastly improve a patient’s chance of success. Contact FHE Health today to learn how we can help you or a loved one overcome addiction in a professional facility with caring staff.