Few mental health disorders have such an impact on physical health as eating disorders, thanks to the unique link between the mental and physical manifestations of these diseases. Naturally, this association is why eating disorder treatment can be so complex and typically requires residence in a clinical setting.
At FHE Health, we understand the struggles of eating disorders. Below is more information about eating disorders, how they manifest, and, most importantly, how effective mental health treatment can promote recovery.
Root Causes of Eating Disorders
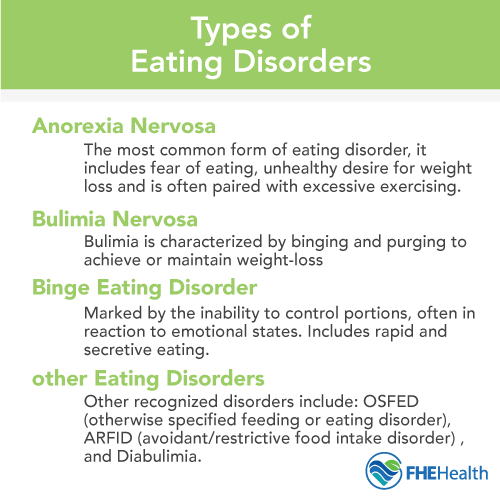
There are many different types of eating disorders, from the ones nearly everyone has heard of, like anorexia, bulimia, and binge eating, to the rarer and lesser-known, like pica and ARFID. To be able to treat any of these disorders, it helps to understand the root causes. As time goes on, medical experts are discovering more and more eating disorders, but as we learn more about them, we’re coming to realize a common thread: eating disorders are diseases that stem from a misappropriation of basic human instinct and function.
Let’s look at some of the forces involved:
Body Image & Societal Pressure
Many factors in a person’s life can stimulate some kind of hyper-awareness of their physical appearance, including societal standards. A person who has received feedback their entire life that they’re too skinny or too fat may develop an eating disorder that comes from an obsession over that feedback.
Basic Human Need
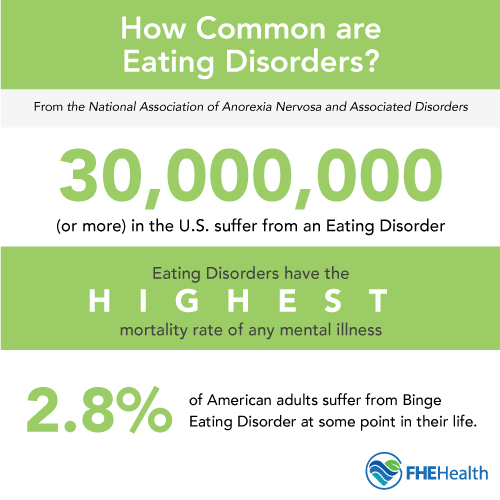
The National Association of Anorexia Nervosa and Associated Disorders (ANAD), a non-profit committed to raising awareness about these focal issues, estimates that at any given time, around 30 million Americans struggle with a documented eating disorder. This may be because, at the most basic level, human life is a cycle of oral nutrition, and it’s easy for these “normal” behaviors to turn into something abnormal.
Psychological and Environmental Factors
Other factors can include, but aren’t limited to: stress, trauma and family history. These elements often interact with a person’s individual vulnerabilities to create a complex web of contributing factors.
Essentially, even though there are different types of eating disorders, and no two people’s manifest in identical ways, several routes tend to be effective in most treatment programs, regardless of the individual disorder. There are also less effective treatments for eating disorders, which we’ll also address.
How FHE Health Treats Eating Disorders
 These are regarded as the most common (and in some cases, clinically proven) techniques in treating eating disorders in adults and adolescents:
These are regarded as the most common (and in some cases, clinically proven) techniques in treating eating disorders in adults and adolescents:
Counseling
Eating disorders are the result of a person’s relationship with food becoming problematic, which can appear physical but is considered part of a group of mental health disorders. This means that, like with many other acute mental health conditions, such as anxiety and depression, traditional therapy and counseling have proven effective.
Types of therapies that have proven successful in treating eating disorders fall in the standard category of evidence-based psychotherapy or “talk therapy.” This allows patients to start to understand the causes of their condition and how to get help with an eating disorder from a health professional. It’s beneficial for patients to talk through their experiences with their condition. When did it start? How did it start? What was going on in their life at the time? Is there anything leading up to the start that could be part of the cause?
These may seem like standard questions, but most eating disorders are defined by the shame they provoke. Many people suffering from this group of conditions do it in silence or even hide it from their friends, family and coworkers. Helping those with eating disorders better understand how control — and often feeling out of control — can play a role in the behaviors and teaching them alternative thought patterns and coping strategies can be very valuable.
Medical Integration With Counseling
It’s also important to explore the fact that an eating disorder may be a mental condition caused by something physical. While this is not extremely common, there have been links found between autoimmune diseases like Type 1 diabetes, Celiac and Crohn’s disease. The common connection could be that these are all diseases in which the body, for different reasons in each case, can’t support certain dietary habits.
It’s unclear exactly what’s at the heart of this link, but it means that patients with eating disorders should also undergo a full medical workup to ensure that symptoms of an eating disorder are not a response to an undiagnosed physical condition.
Medication Options
There are medications that treat the acute effects of common eating disorders. For people with binge eating disorder, and in some cases of bulimia, amphetamines are sometimes used to suppress appetite.
For anorexic patients, drugs used to prompt weight gain, like THC pills and even some antipsychotic meds (anxiety drugs), can be experimented with. However, treating eating disorders with medications shouldn’t be looked at as a sustainable, long-term solution.
Natural Options
What can be a more sustainable solution to a variety of eating disorders is some natural treatments, especially when used in conjunction with counseling. These often involve lifestyle changes, most notably, changes in diet. This may seem fairly obvious, after all, people with eating disorders are working towards a goal involving healthier eating habits, but it’s actually a little more complicated than that.
For example, anorexia commonly results in malnutrition, negatively affecting things like bone density and the normal development of organ systems that aren’t getting the vitamins and minerals needed to stay healthy. In this sense, eating disorders can be part of a vicious cycle: a patient’s eating habits are abnormal due to their condition, and as they continue with these habits, they become less and less healthy.
Diet is strongly linked to mental health, meaning that as a person becomes less and less nourished, their system doesn’t have the tools to address the underlying issues with their mental health. That’s why a common treatment option for eating disorders is what we call “nutritional therapy,” also known as nutritional counseling, simultaneous with traditional psychotherapy.
Can Eating Disorders Be Cured?
Treating an eating disorder is a lot like treating addiction and other mental and behavioral health issues. Once you’ve slipped into a lifestyle you can’t control, you’ll always be at risk of a relapse. Former patients with eating disorders can easily revert to their old lifestyle because their condition involves a very routine human behavior.
That’s why it’s important to resist becoming complacent in recovery, even when your disorder has been in remission for a long time. If you or a loved one has struggled with your eating habits in the past, don’t forget it or feel like you can slip back into old habits “just this once.” Just like people in recovery from substance abuse, you may only be one day away from where you started.
Many people choose to rely on a support group to remind them where they’ve been and the strategies they’ve developed in their “sobriety” (so to speak). The good news is that since eating disorders are so common, there are plenty of options for local and regional group meetings to meet people in similar places to where you’ve been and where you are now.
How Are Eating Disorders Treated?
Initial treatment is highly focused on changing behavioral patterns along with anxiety related to eating, weight gain, and body image. This is most effective in treatment-specific care that monitors and holds patients accountable for behavioral change in a highly structured level of care that addresses and adjusts behavioral patterns.
Once this highly structured level of care has been completed, continued care to work on the psychiatric, personality, and mood issues is important for patients to be able to learn self-management for stability, develop new coping skills, and demonstrate self-control while still living with the mood issues that often trigger the compensatory behaviors evident in eating disorders.
While FHE Health does not provide the highest, most intensive level of care for eating disorders, we offer nutritional interventions and address underlying psychiatric, relational, and personality issues while a patient is gaining the ability to function and learn how to deal with discomfort, stress, and conflicts that are precedents for eating disorder behaviors. Together, our clinical, nutritional, and psychological eating disorder programs in Florida help our patients learn and demonstrate appropriate behavioral responses that will lead to the successful management of an eating disorder over time.








