
Neurostimulation, a technique that involves direct electrical, magnetic and/or other vibrational stimulation to the brain, has been effectively treating mental illnesses like depression for decades in Europe, Australia and other parts of the world. In the United States, however, the treatment is not yet considered mainstream, and FHE Health is one of very few (if any) rehab facilities in the U.S. that offer it. In fact, for a number of years our Neurorehabilitation Program has been using various forms of neurostimulation and other neuroscientific interventions to treat addiction and other mental conditions.
Recently, in an effort to better serve our patients and more fully understand the effects of neurostimulation on patients’ recovery, FHE Health conducted research into how patients were responding to the treatment. Director of FHE Health’s Neurorehabilitation Program Dr. Nicholas Dogris, Ph.D., led the study. He set out to quantify and analyze the impact of neurostimulation on the recovery of patients with addictions to opiates, benzos and stimulants.
In an interview this month, Dr. Dogris explained what he and his research team found, and why patients with substance use disorders have reason to be more hopeful than ever about their prospects of recovery, thanks to this cutting-edge treatment…
How Neurostimulation Improves Detox and Treatment Outcomes for Opiates, Benzos and Stimulants
 How does neurostimulation impact people who are going through detox for opiates, benzos and stimulants? (Opiates, benzos and stimulants are the most common addictions treated at FHE Health.) That was the question with which Dr. Dogris first introduced neurostimulation to FHE Health. It also is what guided his research into patient outcomes.
How does neurostimulation impact people who are going through detox for opiates, benzos and stimulants? (Opiates, benzos and stimulants are the most common addictions treated at FHE Health.) That was the question with which Dr. Dogris first introduced neurostimulation to FHE Health. It also is what guided his research into patient outcomes.
Dr. Dogris wanted to know whether a form of neurostimulation known as transcranial alternating current stimulation (tACS) would impact patients’ EEG tests. (An electroencephalogram is a non-invasive recording of the brain’s electrical patterns, and is used to diagnose all sorts of conditions, from seizures and concussions to headaches, sleeping problems and mental health disorders, including substance addictions.)
Dr. Dogris had other questions, too, about neurostimulation’s effects:
- Would it improve patients’ sleep quality?
- Reduce anxiety?
- Decrease symptoms of depression?
- And, of course, in the same vein as an abundance of data already showing the safety of neurostimulation … would it have any adverse effects on our patients? After all, “Do no harm,” was, and is the number one imperative.
How Neurostimulation Changes the Brain – A Lesson in Neurosplasticity
 Before addressing the study’s results regarding patient outcomes, Dr. Dogris provided a short lay tutorial about how neurostimulation changes the brain. He explained that neurostimulation involves the application of an anode (a positively charged electrode) and a cathode (a negatively charged electrode) to the brain.
Before addressing the study’s results regarding patient outcomes, Dr. Dogris provided a short lay tutorial about how neurostimulation changes the brain. He explained that neurostimulation involves the application of an anode (a positively charged electrode) and a cathode (a negatively charged electrode) to the brain.
The anode, when applied, increases the brain’s blood flow, “which is really good for detoxing,” in Dr. Dogris’ words— “because you need to get [the addictive substance(s) out of your body.” “Wherever you put the anode,” he added, “glutamate drops … Glutamate is the fuel for cells, so the brain starts soaking it up and it will soak it up so quickly that your overall glucose level will drop.” (In other words, brain cells kick into a higher gear of neuroplasticity where self-repair happens more quickly.)
Meanwhile, the cathode creates more of the neurotransmitter GABA. GABA regulates anxiety and promotes relaxation, in addition to a number of other functions.
Here’s how Dr. Dogris described what happens on the cellular level to a brain that is receiving neurostimulation:
The brain has calcium and sodium ions in cells called “glia” or “astrocytes,” which are the glue that glues the brain’s limbic system to its upper cortex. They determine the wiring of your brain. In a healthy brain, they engage in neuroplasticity and help the brain remain healthy. In a brain that’s not healthy, they get stuck and don’t change.
When we apply electrostimulation, on a global level all of the calcium and sodium ions begin to surge and the brain enters into a form of neuroplasticity and starts to change and regulate itself.
Such results would not have been achievable “in the old days of neurofeedback,” when “you couldn’t do this … but with neurostimulation you can make this happen.”
How tCS Can Reduce Pain – Hope for Patients with Acute and Chronic Pain Issues
In addition to hastening the brain’s own capacity for healing and self-repair, neurostimulation can relieve pain. Dr. Dogris explained that the brain has two hubs known as the anterior cingulate cortex (ACC) and posterior cingulate cortex (PCC): the ACC is “sympathetic,” meaning that “when it’s active you’re alert;” and the PCC is “parasympathetic,” meaning that “when it’s active you’re relaxing.”
These two hubs, the ACC and PCC, are “tied together by the pain network … if you have an opioid addiction and you’re supplementing opioids to control pain, this system is what you’re impacting.”
But with neurostimulation, “we apply electrodes around these hubs (the ACC and PCC) to make them switch and the brain will follow the stimulation.” The result: suppressed pain and a decrease in pain sensations.
How the Study Worked
The study tracked five different groups of FHE Health patients. They included one group of 52 opioid patients, one group of 100 benzo patients, one group of 46 stimulants patients (in recovery for meth and cocaine); one control group of 21 patients; and one neurofeedback- only group of 45 patients.
To remove unnecessary variables, all of the patients in the study were detox patients who also were receiving medications during a medically supervised withdrawal. Each of them received an EEG upon admission and then 5-7 days later. Those groups that received tACS got one daily 30-minute session administered across a six-day detox taper.
Study participants were asked to fill out the PHQ and GAD-7, two nationally recognized surveys in the mental health field, about their depression and anxiety symptoms.
How Neurostimulation Improved Recovery from Opiate, Benzo and Stimulant Addictions
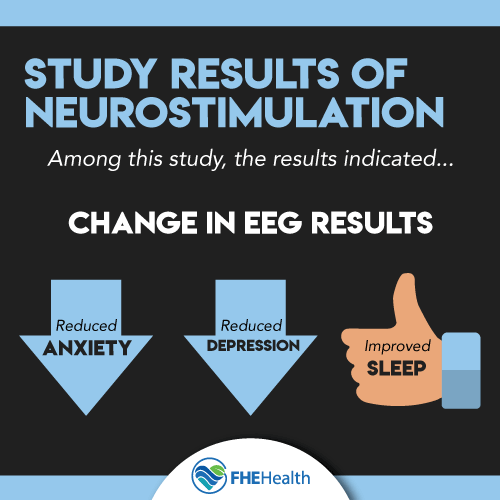 In the end, what Dr. Dogris found was that neurostimulation significantly:
In the end, what Dr. Dogris found was that neurostimulation significantly:
- Changed patients’ EEGs
- Reduced symptoms of anxiety and depression
- And improved sleep.
Also encouraging was the finding that, in alignment with previous conclusions, patients experienced no serious side effects.
Such results are encouraging— and will prompt more research in the direction of exploring the longer-term impact of neurostimulation on the brain, according to Dr. Dogris.
Summing up the findings, he said, “We’re innovating the most effective use of neurostimulation technology in a substance abuse setting that’s above and beyond what’s typically done in detox centers, and we’re achieving significant changes— not only in the brains of these people, but they report their symptoms have dropped significantly.”
Learn more about our Neurorehabilitative Services.






