The coronavirus is raising Americans’ susceptibility to anxiety and depression and making more people anxious and depressed. That’s an inescapable conclusion from recent revelations about the mental health impact of the COVID-19 pandemic and its rippling effects across American society.
It’s not hard to see why the coronavirus is taking a toll on mental health and precipitating higher rates of depression. Fears of infection. Grief over loved ones who have died. Sudden job loss. Record levels of loneliness and isolation. Together, these factors make understanding clinical depression, its signs, and how to get treatment, of paramount importance to every American…
Coronavirus and Depression – The Link and the Statistics
 Coronavirus and depression are now an interlocking epidemic in this country. For one thing, depression is associated with exposure to infectious diseases, according to a study in the journal Psychiatric Research. Stress, too, is a major risk factor for depression. (And many Americans are experiencing more stress now than they have in an entire lifetime.)
Coronavirus and depression are now an interlocking epidemic in this country. For one thing, depression is associated with exposure to infectious diseases, according to a study in the journal Psychiatric Research. Stress, too, is a major risk factor for depression. (And many Americans are experiencing more stress now than they have in an entire lifetime.)
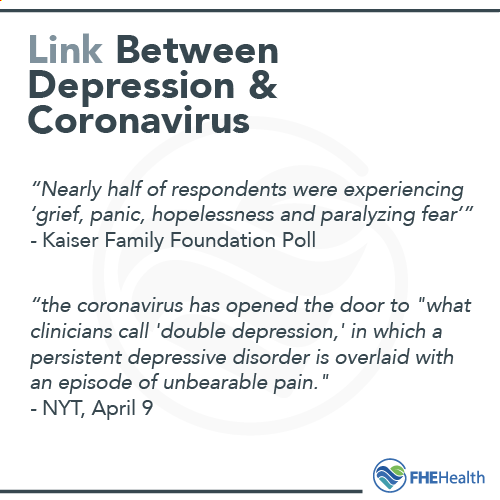
Emerging statistics reinforce the picture that coronavirus-induced depression is both real and widespread:
- A new poll from the Kaiser Family Foundation revealed that nearly half of respondents were experiencing “grief, panic, hopelessness and paralyzing fear,” according to an April 9 op-ed in the New York Times. These (and other) symptoms can indicate clinical depression.
- The same article—by a professor of medical clinical psychology at Columbia University who opened up about his own struggles with depression—went on to note that the pandemic has “catapaulted” a whole, previously uninitiated group of people into depressive and other disorders. Worse yet, for those already suffering from major depressive disorder, the coronavirus has opened the door to “what clinicians call ‘double depression,’ in which a persistent depressive disorder is overlaid with an episode of unbearable pain.”
- Among people who are quarantined for infectious disease, rates of traumatic stress disorders, (which is heavily associated with anxiety and depression), are especially high. Nearly 29 percent of people quarantined during the SARS outbreak of 2003 reported experiencing traumatic stress, according to a February 2020 study in the journal Lancet.
Coping with Depression During COVID-19
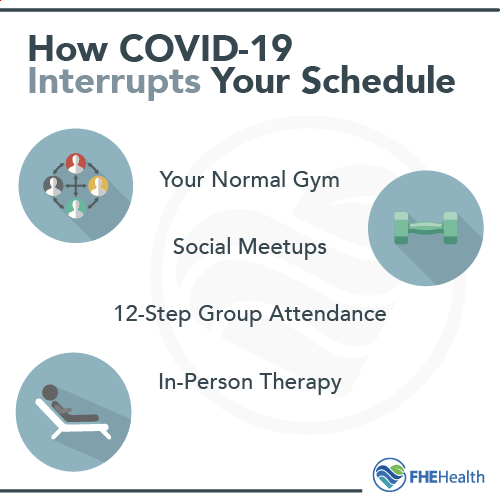 Coping with depression at any time can be tough. Coping with coronavirus-induced depression can be especially difficult. That’s because many of the built-in supports that once were there before the outbreak of COVID-19 are now no longer available or tougher to access:
Coping with depression at any time can be tough. Coping with coronavirus-induced depression can be especially difficult. That’s because many of the built-in supports that once were there before the outbreak of COVID-19 are now no longer available or tougher to access:
- The gym where you once worked out
- The coffee shop where you met up with friends
- The 12-step group that you attended weekly
- The fulfilling job and sense of camaraderie and purpose that it gave you
- The therapist you once saw in person for regular check-ins
- The park where you and your kids used to go to play and connect with the outdoors
For so many of us, these features of pre-coronavirus life played an antidepressive-like role. Many of us, who prior to the coronavirus had never experienced clinical depression, took these things for granted. Others of us, who had learned how to live with depression or another mental health condition, knew these things were essential to our mental health.
Suddenly, almost overnight, these outlets for joy, fulfillment, and positive support disappeared. In their absence, Americans are more vulnerable to first-time clinical depression—or a second, third, or fourth experience of depression. It’s therefore critical to be mindful of what clinical depression is, what its signs are, and how to find immediate help for you or a loved one if you begin to feel overwhelmed.
What Is Depression vs. Clinical Depression?
Everyone faces periodic feelings of loneliness and sadness. These emotions are common and even healthy reactions to the loss of a job or a relationship, stress from work or home or disappointing events. However, for some people, these feelings can last for extended periods of time and become too hard to manage on their own (by sheer will power or other efforts).
Clinical depression is a serious mood disorder that impacts the way an individual feels, thinks and handles daily activities like eating, sleeping and working. Occasional bouts of depression are common, but to be diagnosed with clinical depression, an individual has to have symptoms for at least two weeks.
Recognizing the symptoms of depression is key to knowing when it’s time to seek medical help. Some of the most common symptoms include:
- Difficulty concentrating, making decisions or recalling details
- Feelings for helplessness, worthlessness or guilt
- Pessimism and hopelessness
- Changes in sleep patterns, such as insomnia, waking early or sleeping too much
- Restlessness
- Irritability
- Loss of interest in activities that used to be enjoyed
- Changes in eating habits, including overeating or eating too little
- Persistent feelings of sadness, anxiety or emptiness
- Suicidal thoughts or attempts
In some cases, people who experienced extended periods of sadness develop physical symptoms, including:
- Fatigue and lower energy levels
- Decreased pain tolerance
- Aching muscles and back pain
- Headaches
- Decreased vision
- Stomach pain
- Digestive problems
Different Types of Depression
Clinical depression takes on different diagnosable forms. Major depression (a more common manifestation) is characterized by having symptoms of depression for most days of the week. Generally speaking, doctors diagnose this type of depression when their patients have a depressed mood or a loss of interest in activities that they used to enjoy, in addition to at least four other signs of depression.
Psychotic depression is a disorder in which depression co-occurs with a form of psychosis. For example, a person may experience delusions or hallucinations that typically have a “depressive” theme like illness or poverty.
Persistent depressive disorder is a form of depression that lasts for two years or more. A person living with this disorder may go through some periods where symptoms are relatively mild and others in which symptoms are more intense and disruptive.
When we talk about coronavirus-induced depression, we’re really referring to these three categories of depression: major, psychotic, and persistent depressive. (There are two other types of depression, but these are tied to specific (non-coronavirus) events: Postpartum depression occurs after giving birth, and seasonal affective disorder (SAD) is tied to the change in seasons as sunlight wanes, giving way to winter.)
Risk Factors of Depression
Anyone can be at risk of depression, regardless of their age. While research is ongoing, current research indicates that depression results from a mixture of psychological distress, biological, environmental and genetic factors.
In some cases, depression can result from or co-occur with certain medical conditions like diabetes, cancer, heart disease—or, COVID-19.
Four common risk factors for depression include:
- Physical illnesses or medications
- Major life changes, such as a divorce, the loss of a loved one or moving to a new home
- Trauma
- Personal or family history of depression
Help for You or a Loved One with Coronavirus Depression or Anxiety
The following depression quiz is not intended to make a diagnosis; it takes an unscientific approach that simply provides participants with information about depression, how to recognize its symptoms and how their results stack up to those received by other people.
[qsm quiz=3]
Clinical depression, while highly treatable, can become very serious if it goes undiagnosed. Consult your doctor or qualified mental health professional immediately if you have been feeling down and depressed for at least two weeks.
Common Treatments
Depression is more than a period of sadness, and individuals can’t simply “snap out” of it. It’s a serious condition that requires long-term treatment. For some, treatment may last a few weeks or months. For others, lifelong treatment is necessary. No two people are the same, and there isn’t a one-size-fits-all treatment for depression. In most cases, treatment includes psychotherapy, medication, or a combination of both. If an individual doesn’t experience relief from symptoms with these two types of treatment, their doctor may recommend interventions such as brain stimulation therapy.
Medications
Medications that are used to treat depression are called antidepressants. They help the brain produce, regulate and use certain chemicals and hormones to control stress or moods. An individual being treated for depression may have to try several different antidepressants before they find one that works for them. If a family member is successfully being treated for depression with an antidepressant, that medication will often be considered first.
Antidepressants may take as long as a month to work. Especially as the body gets used to them, they may have some side effects that affect sleep, appetite, and concentration. It’s important that these medications are only taken or stopped under the care of a doctor. Many medications have to be tapered off gradually, or serious withdrawal symptoms may occur.
Psychotherapy
Psychotherapy, or counseling, is another effective treatment for depression. There are several forms of psychotherapy, including dialectical behavior therapy and cognitive behavioral therapy. While in-person meetings aren’t possible during the coronavirus outbreak, many therapists are now providing telecounseling mental health services to accommodate the rising demand. Additionally, many online platforms like Talkspace and DotCom are helping people find the right fit of online therapists for their needs.
Brain Stimulation Therapies
For those with severe depression who are not receiving relief from medication and psychotherapy, brain stimulation therapies may be another option. Electroconvulsive therapy is the best-studied brain stimulation therapy and has a long history of use. Newer therapies include deep brain stimulation and high frequency pulsed electro-magnetic stimulation therapy, both of which show great promise for treating depression. These procedures are painless, non-invasive, and can be performed on an outpatient basis.
Getting Diagnosed with Depression
To effectively treat depression, it’s important to seek care from a licensed mental health professional. While many people attempt to ignore their symptoms and hope they resolve on their own, studies have shown that symptoms of depression only progress in severity when left untreated. The high rates of suicide in this country illustrate just how tragic mental health outcomes can be.
Meanwhile, anyone affected by depression needs to know that safe and effective treatment is available now. Because treatment for depression and other mental health disorders is an essential service during a coronavirus outbreak, providers like FHE Health are open and receiving patients. For help with questions about depression or any other mental health illness or concern, call us today at 1-866-534-3586. We would be happy to help in any way we can.
See More Resources on our Remote Recovery Toolkit