
College students were already the most susceptible to mental health disorders. Their risks are higher this World Mental Health Day. Learn why from an expert at the National Alliance on Mental Illness (NAMI) and—in the theme of World Mental Health Day—invest in their mental health, with this handy self-help tool, “6 Things to Remember When You Feel Really Anxious or Depressed.”
These recommendations come from a mental health expert at the National Alliance on Mental Illness (NAMI), who shared them in observation of “World Mental Health Day,” as part of a fuller interview. Catch the full interview.
2020 is when two public health crises collided. One of them—a record-breaking, mental health epidemic—hit college students especially hard.
Just ask Sandra Cumper, who has been working in the mental health field for more than two decades. She’s the executive director of NAMI Broward County in Florida. NAMI (which stands for “National Alliance on Mental Illness”) is the nation’s largest grassroots organization dedicated to bettering the lives of people living with mental illness.
2020 a Perfect Storm of Mental Health Risk Factors
Cumper often tells families that the college and young adult years (ages 18 to 35) are when many people first experience mental health symptoms (and in this sense college students are more susceptible to anxiety, depression, and other disorders). But 2020 has stood out as markedly worse, according to Cumper, who recently noticed a lot of families calling in to say their college-aged child was experiencing “such dire issues, not knowing what to do or where to turn.” (And, “students themselves were calling in.”)
“A lot of these kids were college and high school students,” Cumper said, in an interview to mark “World Mental Health Day” (Oct. 10). “I started wondering about this.”
That’s when it occurred to Cumper that the pandemic had struck right on “the cusp of spring break and final exams”—so “you’re talking about the stress, anxiety, and anticipation for the spring break… Right in the midst of this, the pandemic hit, and students were asked to do things they weren’t used to, like stay inside.” The ensuing isolation was especially hard when “young people don’t do very well with isolation” and “need to be out and about.”
Meanwhile, college students have also been experiencing unprecedented levels of uncertainty: “Kids were working. They had internships. They had future plans, and almost overnight these disappeared, Cumper observed. “They’re thinking, ‘Will I ever be able to do the things I want to do, if everything seems uncertain now?’” Magnifying that uncertainty and social isolation—many of them weren’t able to access mental health services at the time,” and “delayed care only promotes long-term issues.”
The overall impact has been a “sense of grief, loss, and disbelief” when many college students “can’t really wrap their minds around what is happening … It’s a sense of ‘how can I make a difference? I have been moving forward with an education and seeing a future but now my future seems so dark.’ It’s a sense of ‘Can I really catch up and get back to finishing what I started?’”
Other Mental Health Strains in College
These questions and concerns would be enough to deal with on their own; but there are the other more familiar stressors that usually confront a young person embarking on newfound independence and college life. Cumper was quick to point out that first-year students are “coming from different environments, and they’re expected to merge into this one society as college students … They have to start developing new friends, share rooms with total strangers, interact with new cultures, new experiences, new foods, new thinking.”
Mental health can suffer when “you’re not equipped or prepared for these challenges and new issues,” Cumper said. “With added stress, increased levels of anxiety, feelings of inferiority …. plus, being genetically predisposed to mental health issues, symptoms associating with mental illness can emerge at this stage.”
How Common Are Mental Health Symptoms in College?
Very. 63 percent of college students in the U.S. experienced “overwhelming anxiety in the past year,” according to a 2018 survey by the American College Health Association, Harvard Medical School reported. Meanwhile, “30 percent of college students reported ‘feeling so depressed that it was difficult to function,’” in a report by the National Institute on Mental Health (NIMH).
Both of these reports appeared well before the mental health repercussions of a global pandemic began to set in—meaning this year college students could face a greater chance of experiencing mental health symptoms than not. For Cumper, this reality underlines the importance of mental health awareness: “As a community, we need to prepare young people to go into the great, blue yonder and help them understand they’re entering into a new zone where there are these issues they’re going to face and that need support.”
Tips for Taking Care of Your Mental Health + A Handy Resource That Helps
Mental health symptoms are like other conditions that need prompt medical attention. Cumper recommended paying close attention to your symptoms and—as you would with a physical condition like a heart issue—consulting the right medical specialist (in this case, a psychiatrist). Talk therapy can be healing, too, Cumper said. She also suggested getting involved in a “NAMI on Campus” chapter—if there’s one at your school. (Entirely student-run, these groups provide a safe outlet for talking about mental health concerns and accessing support from peers and other resources.)
Remember anyone can experience a mental health disorder. Keep this free resource on hand just in case. Whether it’s you, your roommate, or your friend, you could be saving a life.
6 Things to Remember When You Feel Really Anxious or Depressed
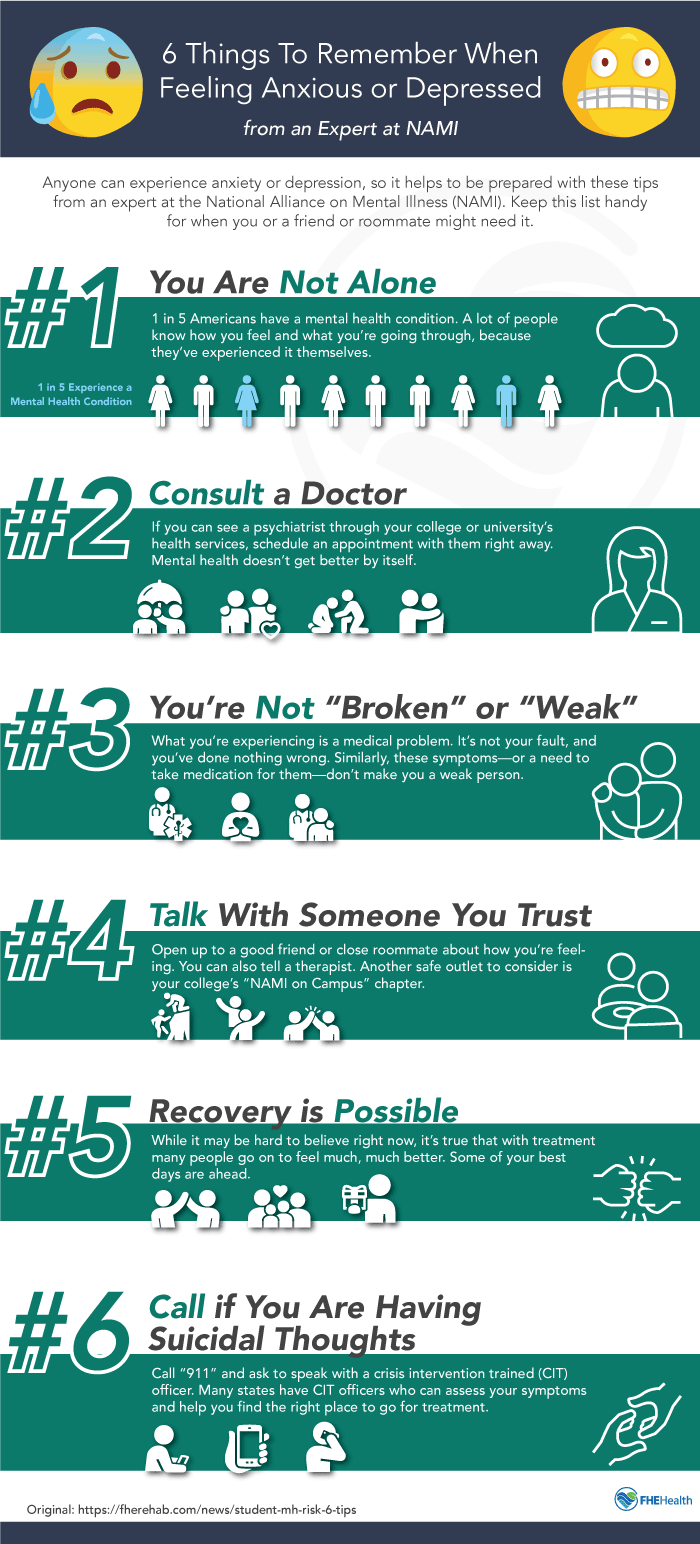
Since anyone can experience anxiety or depression—at any time—it helps to be prepared. These tips from a national mental health expert are helpful preparation and can remind you what to remember when you’re feeling really anxious or depressed and might forget.
Keep this list handy so you can refer to it if you need to: Take a picture of it with your phone; post it on your dorm room wall; or, save it in your desk or purse for when it might come in handy….
- You’re not alone. 1 in 5 Americans have a mental health condition. A lot of people know how you feel and what you’re going through, because they’ve experienced it themselves. There is a whole community of people who can relate.
- Consult a doctor immediately. If you can see a psychiatrist through your college or university’s health services, schedule an appointment with them right away. Mental health doesn’t get better by itself. Seek help early so you can start feeling better as soon as possible.
- You’re not “broken” or “weak.” What you’re experiencing is a medical problem. It’s not your fault, and you’ve done nothing wrong. Similarly, these symptoms—or a need to take medication for them—don’t make you a weak person.
- Talk with someone you trust. Open up to a good friend or close roommate about how you’re feeling. You can also tell a therapist. (If you don’t have a therapist, you should be able to find one through your college’s health and/or counseling services.) Another safe outlet to consider is your college’s “NAMI on Campus” chapter.
- Recovery is Possible While it may be hard to believe right now, it’s true that with treatment many people go on to feel much, much better. Some of your best days are ahead.
- If you’re having suicidal thoughts or impulses, call “911” and ask to speak with a crisis intervention trained (CIT) officer. Many states have CIT officers who can assess your symptoms and help you find the right place to go for treatment.






