
This article has been reviewed for accuracy by our peer review team which includes clinicians and medical professionals. Learn more about our peer review process.
FHE Health’s new Mental Health Program recently opened its doors for the very first time. Dr. Michael Jochananov directs the program, which treats people whose primary diagnosis is a mental disorder. Last week, he took part in a wide-ranging interview that answered frequently asked questions about mental health treatment. (Tune in for the upcoming second installment of that interview when Dr. “J,” as he’s affectionately called, will address more common concerns such as “Does therapy work?”)
In this week’s segment of the interview, Dr. J. talked about his role and vision for our Mental Health program and discussed the range of mental health services it offers. He also shared some insights into what defines quality treatment, as helpful pointers for people who may be looking for mental health services they can trust.
What’s the Role of Our Director of Mental Health Program?
In his new role directing FHE Health’s Mental Health Program, Dr. J is responsible for building the new program from the ground up and for managing and overseeing the implementation of mental health services, including the supervising of staff and patient care. This is no small job. Consider the wide range of patients who are treated in the program, for example:
- Mental Health patients often have the more garden-variety anxiety, mood and/or trauma disorders.
- They also may have rarer and more serious conditions, such as bipolar and psychotic disorders.
- In many cases they have a secondary diagnosis of substance abuse.
Dr. J. doesn’t blink at even the most severe of these cases, maybe on account of experience: For many years prior to joining FHE, he was the clinical director of a long-term treatment center for teens suffering from serious mental illness; now, as an extension of his role with FHE, he will be sharing that expertise via in-service mental health trainings on issues like suicide, homicide, and mental health signs to watch for.
What Range of Mental Health Services Do We Offer?
Naturally, with such a wide range of mental health diagnoses, patients will benefit most from a robust offering of diversified mental health services:
- Individual therapy – Patients can have daily check-ins with their primary therapist and meet with them in a longer, once-weekly individual session.
- Group therapy – Group sessions, led by therapists, occur daily, allowing patients to draw support from peers with similar challenges.
- Family counseling – “The goal is to get [the patient] reintegrated within the community,” Dr. J. explained. “Individuals’ mental health disorders can have a vicarious effect and cause trauma on family, and family members struggle with supporting these individuals as well.”
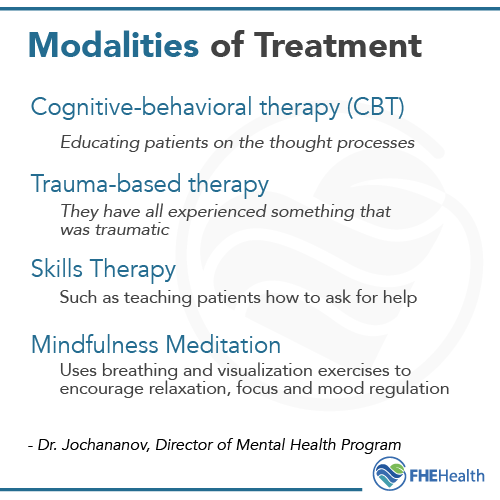
In addition to these various modes of therapy, patients can choose— (in collaboration with their therapist)— from a range of therapeutic “modalities” or approaches to decreasing mental health symptoms:
- Cognitive-behavioral therapy (CBT), in which we’re “edtucating patients on the thought processes” that are aggravating how they feel and act
- Trauma-based therapy, meaning “a focus on trauma” given how universal trauma is among these patients, according to Dr. J. “They all have experienced something that was traumatic,” he said.
- Skills therapy, such as teaching patients how to ask for help
- Mindfulness meditation that uses breathing and visualization exercises to encourage relaxation, focus and mood regulation
These clinical approaches, in combination with medication management, can be very effective at decreasing a patient’s symptoms and providing them with tools they can use to successfully manage their condition back in daily life.
“We want to help set patients up with coping mechanisms that they actually can use at school, work or other social situations,” as Dr. J. explained.
Supplemental services—neurofeedback, yoga, massage therapy, acupuncture—are among the other mental health services that FHE offers. Dr. J. noted that every patient receives a brain scan, and this mapping of areas of neurological dysfunction helps them better understand and accept their condition.
“Genuine interactions are important. Being supporting, accepting and consistent for patients is critical,” Dr. J. said, so “non-structured interactions with non-clinical staff are also a range of services that we provide.” In this sense, housekeeping and other non-clinical employees are instrumental in the healing process also. Or, as Dr. J., put it, “It takes a village to help treat people.”
What Defines Quality Mental Healthcare?
As the director of FHE’s Mental Health Program, Dr. J. spends a lot of time thinking about the quality and outcomes of the therapeutic services we provide. At the top of the list of factors that distinguish effective treatment? “You have to have people who are absolutely dedicated to what they’re doing,” said Dr. J.:

We get to see people at their worst, so we need people who are dedicated, non-judgmental and accepting. This needs to be a trauma-informed environment from the root to the fruit with people who are dedicated to these patients’ well-being. Our staff need to have the knowledge and expertise for working with this population— and continuing education, knowledge and experience about what our folks are struggling with.
“An integrated model for mind and body” is also on that list of factors that define quality care for Dr. J.— hence an emphasis on talk and medication therapies in combination with other holistic interventions.
Third, Dr. J. touted the importance of concrete “benchmarks, so we can see our areas of progress and growth.” Here he was speaking collectively of patients and staff, both of whom need an ability to “celebrate the small victories.” And, by “small victories,” he was referencing the “everyday” tasks in which a patient may gradually (or suddenly!) reveal incremental but observable progress and a reduction in symptoms. For example, the patient who is so depressed and can’t get out of bed and who one day starts to get out of bed— that’s a small victory, according to Dr. J.
When added together, “small victories” like getting out of bed in the morning can mean a big quality-of-life difference for people with mental health conditions and shine a light on the often debilitating costs of not getting professional help for a treatable mental illness.
Got more questions about mental health treatment? Tune in for the second and final installment of our interview with Dr. J, which airs next week.






