Post-traumatic stress disorder is a serious mental health condition that someone may develop after experiencing a scary, shocking, or dangerous event such as an assault, a life-threatening vehicle accident or weather event, an active shooter situation, or the death of a loved one. PTSD may also develop after a person sees someone else experience a trauma. Veterans who’ve served in active combat, for example, are vulnerable to developing this condition.
While it’s normal to experience distress after events like these, a person may be diagnosed with PTSD if memories of the trauma are still disruptive to their day-to-day life a month later. Symptoms of PTSD may include:
- Reliving the experience through flashbacks, nightmares, or visual or auditory hallucinations
- Avoiding people, places, or events that trigger memories or emotions tied to the trauma
- Increased alertness, difficulty sleeping, and angry outbursts
- Intrusive thoughts of the trauma or feelings of guilt or hopelessness
PTSD may be evident within a few weeks following the traumatic event, or it may not develop until years later. It can develop at any age, with the National Center for PTSD reporting that about six percent of people will experience this condition at some point in their lives. Symptoms may resolve on their own, especially in those who are able to make their peace with the event, find emotional support from friends and family, and develop healthy coping strategies. However, in most cases, seeking treatment is necessary for the individual’s safety, health, and quality of life.
The Importance of Seeking Treatment for PTSD
While PTSD can be very disruptive, the good news is that it’s treatable. One study showed that seeking treatment for this disorder reduced the duration of symptoms from 64 months down to 36 months. With treatment, about two-thirds of people achieved full symptom elimination. Even those who still lived with symptoms following treatment reported significant reductions in the intensity of those symptoms.
It can be challenging to overcome barriers to seeking treatment, but living with PTSD can be even harder. This condition is associated with a range of complications, including:
- Muscle, joint, and nerve pain
- Digestive issues
- Chronic heart and lung conditions
- Depression
- Anxiety
- Difficulty with personal relationships
- In extreme cases, suicidal ideation or attempts
There are several therapy types for PTSD that mental health care practitioners may use. Exposure therapy, which involves recounting traumatic events, and cognitive behavior therapy, which addresses thought processes that lead to behaviors, are among the most common types of therapy for PTSD. Many counselors incorporate psychodynamic therapy to help clients learn to navigate emotional conflicts. Eye Movement Desensitization and Reprocessing Therapy (EMDR) can also be useful for retraining the brain and helping it to reprocess painful memories.
Is There Medication for PTSD?
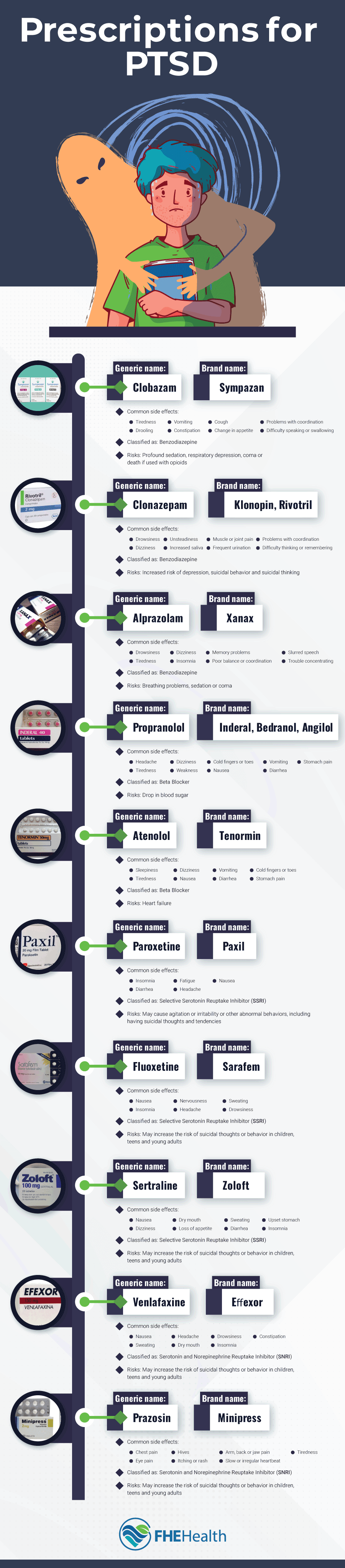
For most individuals, successful PTSD treatment involves a combination of therapy and medication. Although there are no medications that are specifically designed for treating this disorder, there are numerous well-established medications that healthcare practitioners use to treat other mental health conditions such as anxiety and depression that are effective in managing PTSD symptoms. When a medication is used for a condition other than what the FDA approved it for, it’s said to be used off-label.
Many researchers believe that people living with PTSD have different chemical balances in their brains than people without this condition. Certain types of medications used for PTSD work by restoring a proper balance, which can give the individual the mental clarity they need as they progress through treatment.
Selective Serotonin Reuptake Inhibitors (SSRIs)
SSRIs are usually prescribed to people living with anxiety or depression, but they’ve also been shown to be effective in helping control PTSD symptoms. These medications work by preventing the blood from absorbing some of the serotonin the brain produces. As a result, more serotonin stays in the brain. This can have a positive effect on the individual’s ability to focus on everyday tasks, act as a mood stabilizer, promote healthy sleeping habits, and reduce stress levels.
Currently, two medications are approved to treat PTSD, including Zoloft, or its generic sertraline, and Paxil, or its generic, paroxetine HCI. Other SSRIs, such as Prozac, are effective in treating this disorder, though they’re considered to be used off-label if they’re prescribed for this purpose.
Serotonin and Norepinephrine Reuptake Inhibitors (SNRIs)
SNRIs are a class of drugs that prevent the reabsorption of serotonin and norepinephrine in the brain. Norepinephrine, a neurotransmitter like serotonin, increases alertness and energy, helps to balance the mood, and boosts concentration. While SSRIs only keep more serotonin in the brain, SNRIs keep both of these chemicals from absorbing into the blood.
SNRIs are typically used to treat depression, anxiety, and chronic pain, which may make them a better fit for some people living with PTSD than SSRIs. One medication in particular, Effexor (the brand name for venlafaxine) has been found to be effective in people with PTSD.
Benzodiazepines
Benzodiazepines, often simply called “benzos,” are a class of drugs that work in the body’s central nervous system. These medications are depressants, meaning they slow down activity in the brain and nervous system. While SSRIs and SNRIs affect the levels of the neurotransmitters themselves, benzodiazepines attach to the receptors. This makes the receptors less sensitive to stimulation, resulting in a calming effect.
Due to their calming effects, benzodiazepines are typically prescribed for severe anxiety and panic disorders and insomnia, as well as physical problems such as seizures and muscle spasms. They can also ease the symptoms of drug or alcohol withdrawal. Common drugs in this class include Klonopin (clonazepam), Sympazan (clobazam), and Xanax (alprazolam).
While benzodiazepines are safer than ever to use due to lower dosages and the banning of specific types, it’s important to remember that these medications are habit-forming, and there’s a potential for misuse. For that reason, healthcare providers tend to use caution when prescribing them. In most cases, these medications aren’t used on a daily basis but only as needed, and they may not be a good fit for someone with a history of substance use disorder.
Prazosin
Prazosin, sold under the brand name Minipress, is part of a class of drugs called antihypertensives. It works by relaxing the blood vessels to let blood pass through more easily. This medication is typically prescribed to people who have high blood pressure. However, its ability to block the production of norepinephrine, which triggers the body’s stress response, also makes it a good option for those living with PTSD. Some mental health care practitioners may prescribe this medication by itself, but in many cases, they prescribe it alongside an SSRI or SNRI.
Prazosin is generally safe to use, though it may not be good for people who have low blood pressure. To ensure the individual isn’t at risk of a stroke or heart attack, practitioners will closely monitor the patient’s blood pressure.
Beta-Blockers
Beta-blockers are a class of drugs that prevent adrenaline, the hormone that plays a key role in the body’s stress response, from coming into contact with the heart’s beta receptors. Many people use these drugs to manage heart conditions such as high blood pressure, irregular heartbeat, and heart failure. However, doctors may also prescribe these drugs off-label to help the individual manage anxiety and PTSD.
The two beta-blockers that are most often prescribed for PTSD are propranolol and atenolol, which may also be prescribed under their brand names Inderal and Tenormin. These drugs don’t treat the underlying cause of PTSD, but they can help the individual manage symptoms such as increased heart rate, sweating, and shakiness. The individual may still experience times of intense stress, but they may feel less anxious during those times.
Beta-blockers tend to work best when they’re used only when necessary, rather than on a regular basis. It’s also important to note that for some people, these medications actually increase anxiety symptoms. It’s essential for the individual to work closely with the doctor to ensure this medication is beneficial for them.
PTSD can significantly impact the individual’s quality of life for months or years after the trauma itself has resolved. Fortunately, professional treatment that includes a combination of therapy and medication can reduce the intensity and duration of symptoms. To learn more about PTSD treatment, contact FHE today.