
This article has been reviewed for accuracy by our peer review team which includes clinicians and medical professionals. Learn more about our peer review process.
They are the first to respond to any crisis, disaster, or emergency. When COVID-19 struck, they still were first on the scene and have continued to show up—because that’s their job. These “first responders” are America’s heroes.
Watch any Marvel movie, though, and you’ll soon discover that being a hero has its drawbacks. One big one is burnout. First responder burnout is unique: It has its own distinguishing characteristics and can require a different set of preventative and self-care measures as well as treatment responses.
To better understand this distinctive phenomenon and its impact on first responders and their families, we turned to Dr. Sachi Ananda, Ph.D. As the director of a specialized addiction and mental health treatment program for first responders, Dr. Ananda is intimately familiar with first responder burnout and how to recognize, prevent, manage, and ultimately overcome it.
What follows are highlights from the interview, which might just be a source of hope and support for first responders and their loved ones—not just during a pandemic but at any time.
What Is First Responder Burnout and What are the Signs?
 Burnout that goes unrecognized can follow a trajectory leading to drug and alcohol addiction and other mental health conditions. In fact, “If you don’t address the burnout, it will probably lead to more severe symptoms that could become a nervous breakdown,” Dr. Ananda said.
Burnout that goes unrecognized can follow a trajectory leading to drug and alcohol addiction and other mental health conditions. In fact, “If you don’t address the burnout, it will probably lead to more severe symptoms that could become a nervous breakdown,” Dr. Ananda said.
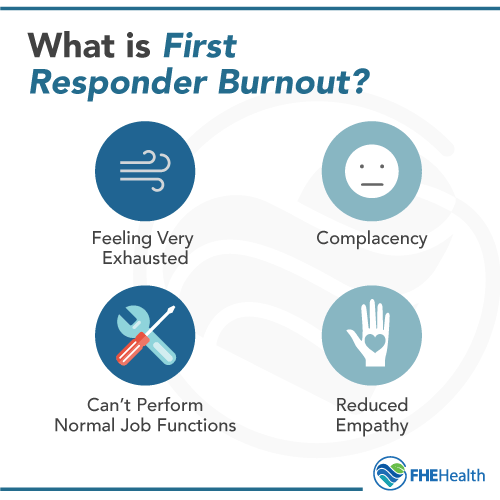
Knowing how to recognize burnout is therefore imperative, but what is first responder burnout and what does it look like? Dr. Sachi described it as follows:
- “Feeling very exhausted and overwhelmed”—because “first responders are working under much more stressful conditions than the average person, and every day is a lot more intense”—and feeling this extreme fatigue “more over a few days than just a bad night or bad call”
- “If there are certain functions on your job that you normally do and now can’t” because “you’re more overwhelmed than usual”
- “Complacency or lack of care about your job”
- “Reduced empathy for the people you’re trying to help”
- “Compassion fatigue”
What Causes Compassion Fatigue in First Responders?
 In the last case, a big cause of compassion fatigue in first responders is “secondary trauma,” according to Dr. Ananda. Secondary trauma occurs from experiencing and observing a traumatic event that is happening or has happened to someone else.
In the last case, a big cause of compassion fatigue in first responders is “secondary trauma,” according to Dr. Ananda. Secondary trauma occurs from experiencing and observing a traumatic event that is happening or has happened to someone else.
Here’s how Dr. Ananda explained it: “It’s when you may not have witnessed or experienced the trauma yourself, but because you help people so much, you almost take on the trauma and stress that they have.”
“Burnout happens on the same continuum with compassion fatigue,” Dr. Ananda said. She added that this continuum keeps going, “from burnout to compassion fatigue to PTSD—although more clinical PTSD is when you’re experiencing certain symptoms, like intrusive thoughts, memories, flashbacks, or doing things to avoid reminding you about the trauma.”
How Common Is Burnout in First Responders?
“Every first responder will experience this in their career at least once,” Dr. Ananda said. The main difference is that some people will be able to rest, take a vacation, and bounce back, while “others who don’t address the burnout will experience more severe symptoms that could become a nervous breakdown.”
Among the first responder treatment population, many “have experienced long-term burnout that requires professional treatment.” Others are retired. They “may not have experienced burnout, but so many years of that accumulated burnout and then retiring … can start to manifest later as chronic disorders like PTSD, depression, anxiety.” Then there are “those who have been injured on the job but their injuries may have been caused by their not taking care of themselves.”
What Are Red Flads to Look for When Considering Stress Management for First Responders?
Much of Dr. Ananda’s job is about helping first responders develop healthy self-care and coping tools that make them more resilient to stress and burnout. One very important aspect of this self-care is recognizing and addressing burnout as early as possible, before a potential spiral into self-destructive or suicidal behaviors. Here Dr. Ananda noted some red flags to watch for, whether you’re a first responder or a family member:
- You experience drastic, negative changes in your attitude toward work.
- You’re excessively irritable around others.
- You wake up and just dread going to work on a daily basis.
- You’ve lost your purpose for doing the work and you really see no meaning in what you do.
- You’ve lost your sense of value.
How Do You Know When to Get Help or Treatment for a First Responder?
These red flags on their own may/may not mean that it’s time to seek help or treatment. For more clarity regarding this question, Dr. Ananda said it’s worth evaluating whether your burnout is causing impairment in your job, social life, or how you relate to other people. If the answer is “yes,” “then it’s very important to seek some professional help so that it doesn’t get worse.”
How Can Self-Care Help First Responders Maintain Their Resilience?
 Self-care and burnout prevention are a team effort. At the very least, that effort should involve both first responders and their families. Sometimes a therapist or treatment provider is also a necessary, if temporary, part of the equation, too.
Self-care and burnout prevention are a team effort. At the very least, that effort should involve both first responders and their families. Sometimes a therapist or treatment provider is also a necessary, if temporary, part of the equation, too.
For first responders who think they may be experiencing burnout, Dr. Ananda had this advice: “Listen to the people around you and if they’re concerned about you.” This advice can be hard to follow. One reason is that “first responders tend to be very strong-minded, which helps them do their job so well—but this can make it harder to listen to other people’s feedback.” The bottom line is that “if there are multiple people worried about you, you should listen to them,” Dr. Ananda said. “Your family and friends will see those symptoms first.”
Be willing to ask for help. That’s Dr. Ananda’s second recommendation for first responders, who typically “go into this line of work with a strong purpose to help” (not necessarily to be helped):
“I think it’s important that people, in general, know that first responders have a super-hero complex sometimes, because they think they can really save the world and forget they’re human with limitations. We can encourage departments to provide that safe environment where it’s okay to ask for help, because everyone as a human being needs to have rest and self-care—and that’s not a sign of weakness. We also can encourage first responders to ask for help.”
For families, Dr. Ananda had the following advice:
- Get educated on the symptoms of first responder burnout.
- Don’t take it personally. Dr. Ananda said this can be a very common trap for loved ones, which is why the above step, getting educated about burnout, is key.
- Talk about ways to reduce stress. These supports and interventions may include reaching out to other family or peer supports for help with financial or emotional burdens.
- Talk with your loved one in a non-judgmental way, avoiding blame or accusations.
- Keep the conversation open and focused on strategizing solutions.
What Are Tips for How to Manage Burnout as a First Responder?
Given the prevalence of burnout among first responders, it’s never a bad idea to be prepared for how to manage it when—not if—it occurs. Dr. Ananda recommended the following self-care strategies for those who may be experiencing burnout:
- Tell someone you trust or talk with a therapist. “It never hurts to see a therapist in my opinion,” Dr. Ananda said.
- Practice meditation or other relaxation techniques.
- Set some clear boundaries about what you can and cannot do.
- Eat healthy.
- Exercise good sleep hygiene.
Burnout can happen to anyone. First responders are especially susceptible, and it’s easy to see why. Ultimately, though, “being able to trust other people to help you through challenges” is key to recognizing and effectively responding to burnout. If you or a loved one is struggling, help is available.
More Resources And Support For First Responder Heroes:
- 7 Reasons First Responders Need Specialized Mental Health Treatment and Support
- The Real Dangers of Fentanyl Exposure for First Responders
- First Responder Mental Health at Heart of New Partnership
- First Responders to the New Haven Overdose Praised by Experts at FHE Health
- 5 Ways to Show Support for First Responders on the 20th Anniversary of 9/11






