Bipolar disorder is a mental health condition that affects mood, impulse control, and ability to interact with others. There are two types and a related disorder, cyclothymia, but they all involve the person experiencing cycles of hypomania (or mania in bipolar 1 disorder) and depression over time. In some cases, the symptoms of bipolar disorder can cause someone to attempt to self-medicate with drugs or alcohol, or the person may engage in substance use when they are hypomanic.
Substance use can also exacerbate mental health conditions, creating the potential for a perfect storm when it comes to bipolar and alcohol use disorder or other addictions. In this article, we explore the link between bipolar disorder and substance use and how the right treatment plan can help you find long-term recovery.
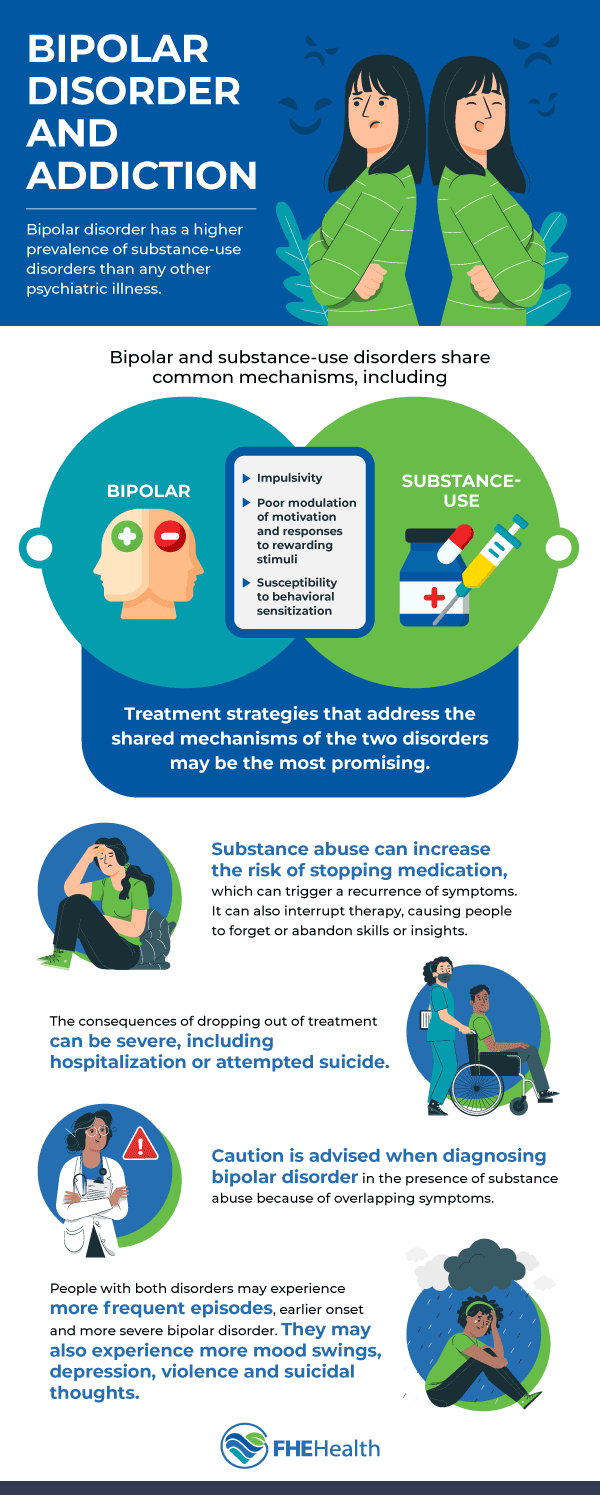
The Connection Between Bipolar Disorder and Substance Use
In the United States, an estimated 2.8 percent of the population has been diagnosed with bipolar disorder, which is over 9 million people. A little over 20 percent of the U.S. population has an alcohol use disorder, and 25 percent are addicted to drugs. An estimated 2.7 percent of those in the United States who were 12 years of age or older had both an alcohol use disorder and a drug use disorder. Perhaps unsurprisingly, there is a good bit of overlap between those with bipolar disorder and those with substance use disorders.
Of those with bipolar I disorder, 40 percent will deal with a substance use disorder at some point in their lives. Alcohol use disorder is more common, with a 58 percent prevalence rate, compared to 38 percent for a drug use disorder. Those with bipolar II disorder are at a slightly lower risk (20 percent lifetime prevalence) of a co-occurring substance use disorder.
So, why is there an overlap between bipolar disorder and substance use disorder? Can drugs cause bipolar, or does having bipolar disorder increase substance use? The answer is a bit of both. While using drugs and alcohol doesn’t cause bipolar disorder, it can exacerbate the condition. It may cause the disorder to come on earlier — it’s most commonly diagnosed in teenagers and young adults — or worsen symptoms. Some of the medications commonly used to treat bipolar disorder can also interact with alcohol and other drugs, which can worsen side effects. The symptoms of bipolar disorder can also make someone more likely to experiment with substances or attempt to self-medicate, as discussed in more detail below.
Why Those With Bipolar Disorder Are More Vulnerable to Addiction
Both depressive and hypomanic episodes can increase the chances that someone with bipolar disorder will use drugs or alcohol.
A depressive episode is characterized by changes in sleeping and eating habits and low mood. The person may start sleeping much more than normal or find falling or staying asleep difficult. Similarly, a person may eat more to distract themselves or may not be interested in eating at all. Depressive episodes in someone with bipolar disorder can involve an extremely low mood, including feeling hopeless or attempting suicide. When someone is in a depressive episode, they may be more likely to use drugs or alcohol to cope with overwhelming feelings or to provoke emotion when they feel numb to the world.
Hypomanic episodes last at least four days and involve an unusually high mood or extreme changes in how the person feels and interacts with the world around them. For example, someone experiencing hypomania may find that they are much more social than normal or have extremely high energy. People often find that they don’t need much sleep or food and may experience racing thoughts and a feeling of being invincible. Hypomanic episodes can increase the risk of substance use because people often have decreased inhibitions and an increase in risk-taking behavior, which can involve experimenting with substances. The feeling of being invincible may also lead people to mix substances or take more than normal, potentially leading to an overdose.
Those with bipolar disorder may also use substances as a way to self-medicate, such as using uppers and downers to manage cyclical symptoms and attempt to achieve a more balanced mood. The stress related to some bipolar symptoms, such as having difficulty in relationships or holding a job, may also drive some people to use.
There is evidence pointing to a potential genetic component to bipolar disorder, and childhood trauma is a known risk factor. Both of these things also increase the risk of substance use disorder, potentially explaining some of the overlap.
Challenges in Treating Co-Occurring Conditions
Co-occurring conditions, commonly known as dual-diagnosis, can make finding an effective treatment plan more challenging because both conditions must be addressed. Treating one can also exacerbate the other. For example, if someone with bipolar disorder has been self-medicating with drugs or alcohol, getting sober without better coping skills in place could worsen their bipolar symptoms. Some of the other challenges for dual-diagnosis treatment include:
- Difficulty getting an accurate diagnosis. Because so many of the symptoms of mental health disorders and addiction overlap, it can be difficult to tell at first what is related to substance use and what is related to another condition. In some cases, a mental health condition like bipolar disorder is only diagnosed after the person has gotten treatment for addiction that didn’t resolve all of their symptoms.
- Potential misuse of medications. Those who are struggling with substance use disorder may misuse the medications the provider prescribes to treat bipolar disorder.
- Environmental triggers. It’s common for people to face some challenges as they return to their normal environment after being treated for mental disorders and substance use. Environmental triggers, such as seeing people you used to use drugs with or going back to a high-stress job, can make it more difficult to avoid maladaptive coping mechanisms.
- Treatment compliance. Those with bipolar disorder can struggle to maintain compliance with their treatment protocol, particularly in hypomanic episodes where they may believe that they are “cured” or no longer need medication or other treatments.
While it’s clear that treating bipolar disorder and substance use disorder together may make things more complex, there are health care providers and mental health teams who work with these situations regularly and are well-equipped to help.
The Importance of Comprehensive Treatment Plans for Lasting Recovery
When it comes to how to deal with bipolar and drug addiction in combination, a comprehensive treatment plan is key. It’s important to work with a health care provider who has experience in dual-diagnosis treatment and the complexities of bipolar disorder itself. Keep in mind that bipolar disorder can’t be “cured.” Instead, those dealing with the condition must have continued treatment, which may include monitoring and adjusting medications, therapy, and lifestyle changes. However, with the proper help and a commitment to ongoing treatment for both bipolar disorder and substance abuse disorder, recovery is possible.