Updated March 28, 2025
Antidepressants are frequently-used drugs that can address everything from bipolar disorder to depression. Of the population over 12 years of age, 13.2 percent has taken an antidepressant in the past thirty days.
With the ability to help millions of people struggling with depression, PTSD and many other conditions, antidepressants can be lifesaving for those who use them. However, as with all drugs, antidepressants can be abused and treatment may be required for those who are dependent.
What Are Antidepressants?
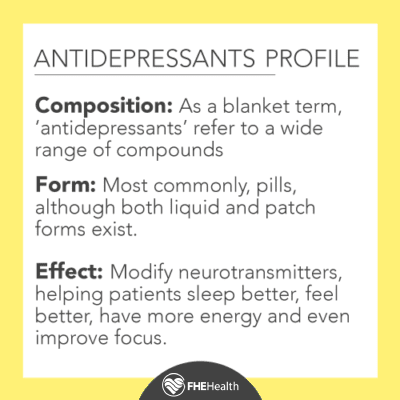 “Antidepressant” is a blanket term that refers to several classes of drug most commonly prescribed for depression or other mental health challenges. Antidepressants come in many different forms, but all major varieties have grown in popularity over the last several decades, in part due to the influx of such drugs that have been released onto the market in recent years, as well as efforts to destigmatize mental health.
“Antidepressant” is a blanket term that refers to several classes of drug most commonly prescribed for depression or other mental health challenges. Antidepressants come in many different forms, but all major varieties have grown in popularity over the last several decades, in part due to the influx of such drugs that have been released onto the market in recent years, as well as efforts to destigmatize mental health.
Antidepressants work by adjusting neurotransmitters within the brain to stabilize mood and emotion. By normalizing the processes for dopamine, for example, it’s possible to help patients to sleep better, feel better, have more energy and even improve focus.
What Kinds of Drugs Are Antidepressants?
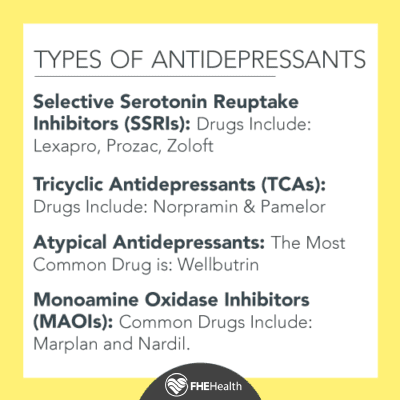 As mentioned, antidepressants aren’t all the same. This category of medication actually refers to several different classes of drugs including:
As mentioned, antidepressants aren’t all the same. This category of medication actually refers to several different classes of drugs including:
- Selective Serotonin Reuptake Inhibitors (SSRIs): As the name implies, SSRIs block the reuptake of serotonin, a neurotransmitter responsible for many complex functions, including promoting cognition, memory, and learning, but most commonly associated with well-being and happiness. Depression is often believed to be connected to a lack of chemicals like serotonin, so increasing levels in the brain can be effective for many patients. SSRIs are referred to as inhibitors as this function does not extend to other neurotransmitters. Common examples of SSRIs include Lexapro, Prozac, and Zoloft.
- Tricyclic Antidepressants (TCAs): Tricyclic antidepressants, also referred to as cyclic antidepressants, are among the earliest forms of medication used to treat depression. As such, they are less common today due to the increased efficacy of other forms of antidepressants, like SSRIs. The functionality of TCAs is similar to that of other similar drugs, acting to regulate levels of serotonin and norepinephrine in the brain. Examples of TCAs include Norpramin and Pamelor.
- Atypical Antidepressants: Atypical antidepressants are drugs that do not fit into the more commonly accepted classes of antidepressants. They function in classes of their own and thus cannot be lumped into groups like SSRIs or MAOIs. Atypical antidepressants still act on neurotransmitters in the brain like serotonin, norepinephrine, and dopamine, but the mechanisms through which this accomplished can vary greatly. The most commonly used example of an atypical antidepressant is Wellbutrin.
- Monoamine Oxidase Inhibitors (MAOIs): MAOIs are antidepressants that inhibit the reuptake of monoamine oxidase, an enzyme that is responsible for removing neurotransmitters like norepinephrine, serotonin, and dopamine from the brain. While somewhat effective, MAOIs have fallen out of favor due to potential interference with other medications and mechanisms for physical health. Those who take MAOIs are encouraged to follow a restrictive diet to reduce the likelihood of high blood pressure. These drugs can also affect other neurotransmitters that control additional functions, causing potentially serious side effects. Doctors may have to customize or adjust care during medical procedures for patients taking MAOIs to avoid critical complications. As such, MAOIs are often the last choice in treating depression. Examples include Marplan and Nardil.
Antidepressants are not instantly effective, with most varieties requiring around six weeks for true progress. Antidepressants also don’t affect everyone in the same ways, so patients may need to try several different medications, or a combination of medications, to find a fit that alleviates symptoms of depression without triggering unpleasant side effects.
How Are Antidepressants Used?
Antidepressants are most commonly prescribed for depression but can be used for a number of different medical conditions. The effects of these kinds of medications on the brain can offer significant improvement in a wide range of illnesses and health issues.
SSRIs are the most commonly used class of antidepressants due to a proven efficacy in conjunction with moderate and tolerable side effects. SSRIs can be used to treat:
- Depression
- Anxiety disorders
- Mood disorders
- Obsessive-compulsive disorder (OCD)
- Attention deficit hyperactivity disorder (ADHD)
- Fibromyalgia
- Menopausal symptoms
- Neuropathic pain
Tricyclic antidepressants may also be used to address some of these conditions, including depression, pain from fibromyalgia, chronic pain and anxiety. Some atypical antidepressants may have additional uses. Wellbutrin is also sold under the trade name Zyban as a smoking cessation aid, while Trazodone is also used to treat insomnia.
Notable Features of Antidepressants
SSRIs
All SSRIs are believed to work similarly by increasing the amount of serotonin in the brain. These drugs are generally the first medication treatment for depression as they are generally highly effective and come with few side effects. Moreover, they are prescribed to treat a wide array of mental health conditions, including:
- Generalized anxiety disorder
- Obsessive-compulsive disorder (OCD)
- Panic disorder
- Bulimia
- Bipolar disorder
- Post-traumatic stress disorder
- Premenstrual dysphoric disorder
Many doctors prescribe SSRIs for off-label uses too such as treating autism, binge-eating disorder, and fibromyalgia. Since SSRIs support the presence of “feel good” chemicals in the brain, they can benefit conditions other than depression. While these drugs do not make the body produce more serotonin, they are able to make sure that present chemical levels in the brain remain at optimum, and when the levels are, the outcome is, generally, improved symptom relief.
Tricyclic Antidepressants
Tricyclic antidepressants work similar to SSRIs, but they tend to come with more side effects and are not as effective for treating depression or other conditions. Some of the side effects these drugs produce include:
- Drowsiness
- Blurry vision
- Reduced blood pressure
- Urine retention
- Constipation
- Dry mouth
Less common side effects associated with these drugs include: sexual problems, increased weight or weight loss, tremors, excessive sweating, and drowsiness.
Unfortunately, these drugs have a lesser impact on serotonin levels in the brain. Those prescribed these drugs should not take them in large amounts or combine them with other types of medications that could affect serotonin levels.
Atypical Antidepressants
Like other antidepressants, atypical ones change the chemistry of the brain and may impact one or more chemical messengers in the brain. These drugs impact serotonin, dopamine, or norepinephrine. However, they achieve their aims differently than other more common antidepressants like SSRIs. Users should also keep in mind that these drugs can cause side effects such as:
- Dizziness
- Dry mouth
- Nausea
- Changes in appetite
- Constipation / diarrhea
- Insomnia
Monoamine Oxidase Inhibitors
MAOIs take time to work and reduce the symptoms of depression like many other depression medications. Unfortunately, these drugs are associated with more side effects, potentially serious side effects. These side effects can include:
- Skin reactions
- Insomnia
- Drowsiness
- Headache
- Nausea
- Dry mouth
- Dizziness
However, the serious side effect that doctors are concerned about is the potential for a drop in blood pressure. Combining certain foods and drinks with MAOIs can be extremely dangerous.
Antidepressants and Addiction?
 Antidepressants are not frequently associated with abuse or addiction. However, the misuse of antidepressants is certainly possible, as evidenced by reports of some people taking these medications in very high doses to achieve psycho-stimulant effects. Even though it is impossible to get high off of antidepressants, some individuals do not understand this and attempt to take high doses. In some cases, patients will choose to increase their own doses in an effort to improve symptoms, creating additional challenges in addressing drug use and management.
Antidepressants are not frequently associated with abuse or addiction. However, the misuse of antidepressants is certainly possible, as evidenced by reports of some people taking these medications in very high doses to achieve psycho-stimulant effects. Even though it is impossible to get high off of antidepressants, some individuals do not understand this and attempt to take high doses. In some cases, patients will choose to increase their own doses in an effort to improve symptoms, creating additional challenges in addressing drug use and management.
Antidepressant dependence is a much bigger risk than these more anecdotal instances of abuse. Using these kinds of medications long-term can indeed create a dependence that makes ceasing use a long and dangerous process. This isn’t always problematic—many people who take antidepressants take them for decades to control disorders that cannot be addressed through other methods—but for others, breaking the habit can be truly challenging.
Physical dependence on antidepressants is in fact very common. Many people end up taking these medications for years after struggling to come off of them. The withdrawal symptoms can be that unpleasant.
Dependence and Long-Term Effects
One reason dependence seems to happen so easily may have to do with how these drugs–or at least the most popular ones—work to achieve their antidepressant effects. SSRIs, which account for an overwhelming majority of antidepressants on the market, block serotonin receptors in the brain. This increases the short-term availability of the feel-good neurochemical but has the opposite effect in the longer term. The brain adjusts by reducing its own production of serotonin. This much lower supply of serotonin in the brain can then increase the user’s chances of a depression relapse and give rise to long-term drug dependence.
Withdrawal is also common with antidepressants, with side effects including:
- Insomnia
- Vivid dreams
- Anxiety
- Fatigue
- Mood swings and irritability
- Muscle aches and chills
- ‘Brain zaps’, or electric shock sensations
- Returning symptoms of depression
To minimize these issues many physicians recommend a slow taper process. However, after long-term use, avoiding any ramifications is not always possible.
Help for Antidepressant Dependence and Withdrawal
Due to the withdrawal process and challenging side effects, quitting an antidepressant cold turkey is often not possible. In these cases, a monitored taper may be necessary. An addiction psychiatrist, who specializes in treating drug dependence, should be able to prescribe medicines and supplements that relieve withdrawal symptoms and support better brain health. A therapist may be able to offer behavioral tips and coping tools for sustaining a healthy lifestyle. For more information about how to address a dependence on antidepressants, contact FHE Health.