Suboxone® is an FDA-approved medication-assisted treatment (MAT) for opiate addiction. When administered with psychotherapy, the medication is associated with better treatment outcomes. Clinical studies have found it to be more effective than a placebo at relieving withdrawal symptoms, decreasing cravings, and reducing risks of relapse during recovery, not just during detoxification but as long-term maintenance.
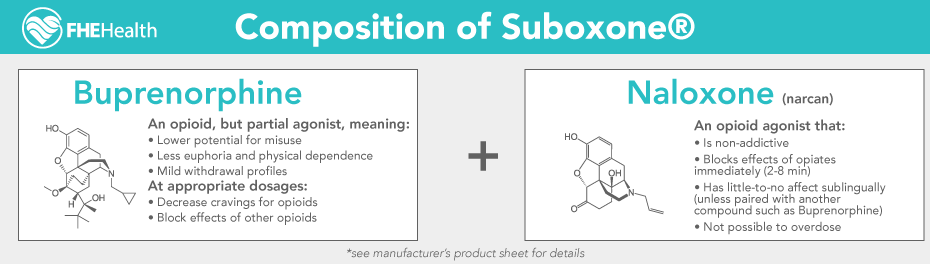
Suboxone® consists of two main active ingredients, buprenorphine and naloxone:
- Buprenorphine has painkilling properties as an opioid, but is a weak opioid agonist, meaning it only partially binds to the brain’s opioid receptors. It therefore cannot produce the same intense high associated with highly addictive opioids like heroin or morphine. Buprenorphine-formulated medications are prescribed by a doctor and often come in the form of a thin, dissolvable sublingual strip or tablet.
- Naloxone, an opioid antagonist, attaches itself to opioid receptors in the brain before opioids can, thereby blocking and reversing opioids’ effects. Naloxone (also known by the brand name “Narcan”) is known for its ability to bring people back from the brink of death after an opiate overdose. When packaged on its own as an emergency treatment for opioid overdose, naloxone comes in two forms, as an injectable or nasal spray.
This combination of buprenorphine and naloxone distinguishes Suboxone® from Subutex. The two medications are often referenced interchangeably when in fact they are different from one another. Subutex contains the partial opioid agonist buprenophine but does not contain the opioid antagonist naloxone.
In the sections that follow, we’ll provide more of an introduction to Suboxone®. We’ll explore how its two-part formulation, buprenorphine and naloxone, can support the detox process in early recovery, and we’ll address some common questions and concerns about the drug.
How Is Suboxone® (Buprenorphine-Naloxone) Dispensed?
Suboxone® can be dispensed as sublingual film strips. These usually come in prescriptions tailored for the length of the detoxification process. (Learn more about the use of buprenorphine-containing products like Suboxone® in MAT.)
During long-term maintenance, Suboxone® prepackaged strips are typically taken daily. The usual single daily dose is 12mg/3mg buprenorphine/naloxone.
How Buprenorphine-Naloxone Works in Withdrawal and Early Recovery
How does buprenorphine-naloxone work to relieve cravings and other symptoms during withdrawal and early recovery?
Someone who is addicted to opiates has likely found that once they stop taking opiates after a period of daily use, withdrawal symptoms quickly ensue. For example, if someone uses a gram of heroin regularly and then suddenly stops cold turkey, they will invariably experience flu-like symptoms (vomiting, shivering, sweating, etc.).
Buprenorphine is administered once withdrawal symptoms have begun; and, because it is a mild opioid, it can produce similar effects to those of opiates. The active amount of buprenorphine is small relative to the amount that someone would be taking to get high, and therefore simply reduces the feelings of sickness that come from abruptly halting opiate use. The ratio of buprenorphine to naloxone is 4:1 (ratio of free bases).
At the same time, the naloxone in Suboxone® is a deterrent to potential misuse of buprenorphine. The presence of naloxone may help to explain why in studies there have been less opioid-related overdoses among people taking buprenorphine-naloxone than a placebo.
How Buprenorphine-Naloxone Works as Long-Term Maintenance
In the world of drug treatment, it is not uncommon to see someone make multiple attempts at lasting sobriety and end in failure, overdose, and, sadly, death. This means that patients with severe opiate addiction may have the option of long-term Suboxone® maintenance. It involves a highly supervised, daily dose that can help them function on a daily basis without resorting to heroin or another opiate drug of choice. The goal of this treatment is to help recovering individuals maintain long-term, permanent abstinence. For many people, too, maintenance treatment for at least six months without overdosing means more peace of mind for their families and loved ones as the patient progresses in their recovery.
The opioid buprenorphine can produce physical dependence and be prone to misuse, although not to the same extent as other opioids. Buprenorphine withdrawal is also less severe than withdrawal from opiates like heroin. Ideally, a patient would be weaned off in progressively lower amounts until they are off the medication altogether. Any withdrawal symptoms during the course of this gradual, medically supervised tapering would be mild. Sometimes non-narcotic medications may be prescribed to relieve symptoms such as fatigue or nausea, if needed.
What Is a Suboxone® Strip?
Sometimes referred to as Suboxone® film, these strips have been approved since 2002 to treat opioid use disorder. The strips are administered under the tongue (sublingually) or buccally (against the cheek). Suboxone® strips are orange and imprinted with a logo and their strength in white ink.
The goal of a MAT such as Suboxone® is to prevent withdrawal and intense cravings for opioids. While taking Suboxone® strips, recovering individuals tend to find it easier to focus on other important aspects of treatment such as their one-on-one therapy or peer group counseling.
Can You Abuse Suboxone® Strips?
Suboxone® strips are not as easy to abuse as a pill or tablet. This makes them preferable for many medical caregivers, who want to minimize the risks of abuse wherever they can.
Taking more than a prescribed dose or taking the strip with other addictive substances, including alcohol, constitutes abuse. Fortunately, the risk of Suboxone® addiction is lower than more dangerous (and deadly) opioids. However, “buprenorphine, like morphine and other opioids […] poses a risk of overdose and death,” according to the Suboxone®’s prescribing information. It also states that “the risk is increased with the abuse of buprenorphine and alcohol and other substances, especially benzodiazepines.”
Suboxone® is not for everyone facing an opioid addiction. For instance, Suboxone® use is not recommended for patients who have severe liver problems or serious respiratory conditions such as asthma.
Is It Dangerous to Take Too Many Suboxone® Strips?
Yes, too much Suboxone® and not taking it as directed can cause overdose. When overdose happens, it is usually when the medication has been mixed with sedatives such as benzodiazepines that can affect breathing, according to Harvard Health in an August 2024 article.
Some people may be at increased risk of Suboxone® addiction because of a medical condition that can affect how the body processes the drug. For instance, people with reduced kidney or liver function are at increased risk for Suboxone® overdose.
The clinical presentation of buprenorphine overdose will present similar to that of opioid overdose, including symptoms such as pinpoint pupils, sedation, hypotension, hypoglycemia, respiratory depression, and death.
Can You Take Suboxone® with Other Drugs?
Suboxone® can have interactions with these drugs, as documented in Suboxone®’s prescribing information:
- Benzodiazepines and other CNS Depressants (including alcohol): Due to the additive effects of these drugs, cessation is preferred. In other words, the effects of the opioid buprenorphine are similar to the effects of benzos and CNS depressants, and should not be combined.
- Inhibitors of CYP3A4: Concomitant use with buprenorphine can increase plasma concentration, resulting in increased or prolonged opioid effects. Consult with your physician to understand the effects of beginning or ending use.
- CYP3A4 Inducers: Concomitant use of buprenorphine can decrease plasma concentration of buprenorphine, potentially resulting in decreased efficacy or onset of a withdrawal syndrome in patients who develop dependence on buprenorphine. Consult with your physician to understand the effects of beginning or ending use.
- Antiretrovirals: NNRTIs, NRTIs and PIs: Studies show significant impact with NNRTIs, some impact with PIs and no impact on NRTIs. As always, consult with your physician and refer to the medication prescribing information.
- Serotonergic Drugs: Serotonin syndrome has been noted from concomitant use. Monitoring is suggested.
- Monoamine Oxidase Inhibitors: Interactions may manifest as serotonin syndrome or opioid toxicity.
- Muscle Relaxants: Combined use with buprenorphine may increase respiratory depression and enhance the blocking action of the relaxant.
- Diuretics: Like many opioids, it can reduce the efficacy of diuretics.
- Anticholinergic Drugs: Their combined use may increase risk of urinary retention.
Risks of Suboxone®
While Suboxone® has saved thousands of lives from overdose and severe opiate addiction, its use can still be somewhat controversial in the recovery community. The fact that it keeps people off worse drugs, alleviates withdrawal symptoms, and can prevent overdose make it a valuable tool in the fight against the opiate epidemic.
Even so, while it is less addictive than other opiates, it is not without some risk of dependence and addiction. Some people may take Suboxone® for years at a time and then struggle to get off of it because of the withdrawal symptoms that can occur. Tapering off Suboxone® can be difficult, depending on the person.
Some in the recovery community view taking a MAT like Suboxone® as simply trading one drug for another. They do not view the use of buprenorphine as “true sobriety” and may consider it an obstacle. Many people believe that a long-term residential treatment program with complete sobriety is the only way to achieve true recovery. They insist that a treatment program helps change a person’s mind, body and spirit, which is necessary for a life transformation away from drugs. Still, it is hard to argue against buprenorphine for people who have tried treatment multiple times and cannot stay sober. The fact that people can take Suboxone®, avoid overdosing, and avoid using street drugs seems like a step in the right direction.
Only a qualified doctor can prescribe Suboxone® on the basis of whether there is a medical need for it, and it should always be taken with medical supervision under the care of a professional.
If you are considering a medication-assisted treatment for yourself or a loved one, reach out to FHE Health. This treatment method has helped many people successfully achieve recovery. Our compassionate counselors are available 24/7 to answer any questions.