In medicine, there are four key vital signs: temperature, pulse, respiration and blood pressure. However, in many ways, pain is often seen as a phantom fifth vital sign. After all, a doctor’s oath quite literally states “First, do no harm,” and what is more harmful than pain? As such, keeping patients pain-free and comfortable has become a central indicator of success in a clinical environment.
Most patients, particularly those who had an accident or a procedure, are asked about pain. Unlike stats like heart rate or respiration, there’s no quantitative way to assess pain, and a patient’s perception is the only way to gauge the reality of a situation. When mismanaged or incorrectly interpreted, a simple question — like “On a scale of one to 10, how much pain are you in?” — can lead to serious ramifications.
The realities of the opioid epidemic are no secret to anyone. In virtually every state across the U.S., overdoses are on the rise, leading to an onslaught of premature deaths across virtually every age, race and income level. While many social outreach programs and harm reduction campaigns are targeting addiction and abuse at the source, it’s equally important to understand the driving forces behind the trends we are seeing today. One of the largest culprits? Prescription pain medication and the willingness of doctors to utilize pills as the first line of defense in place of alternative strategies.
Pain Management and the Opioid Crisis
 Pain management is a medical specialty that requires a fellowship after the successful completion of a residency. While graduate medical education in pain management is open to those who complete a number of different training programs, most practitioners are board-certified in anesthesiology. As the name implies, pain management as a field is dedicated to managing chronic and acute pain in patients for any number of reasons, including post-surgical recovery, neuropathy and orthopedic issues.
Pain management is a medical specialty that requires a fellowship after the successful completion of a residency. While graduate medical education in pain management is open to those who complete a number of different training programs, most practitioners are board-certified in anesthesiology. As the name implies, pain management as a field is dedicated to managing chronic and acute pain in patients for any number of reasons, including post-surgical recovery, neuropathy and orthopedic issues.
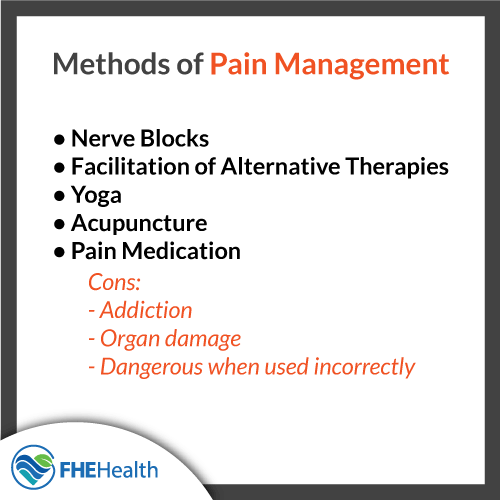
Pain management can be addressed in several different ways, including nerve blocks and the facilitation of alternative therapies, like yoga and acupuncture. However, the default for most physicians is the prescription of pain medication, like oxycodone and hydrocodone. When used appropriately, these kinds of drugs can be very effective in controlling and minimizing pain, but this process is not without complications. From addiction to organ damage, pain medicine can be dangerous and debilitating when used incorrectly or over a long period of time.
The Current Role of Prescription Pain Medication
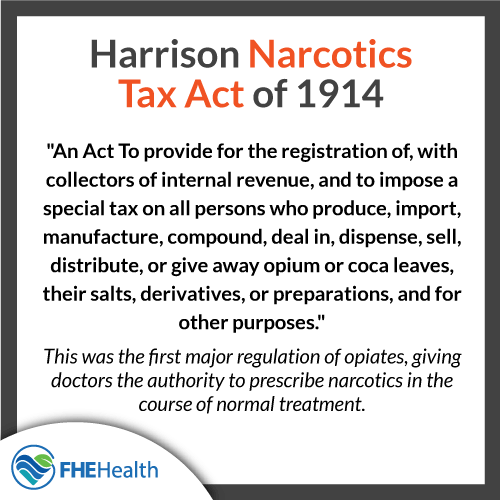
The use of opiates in medicine has a long, rich history in the United States and around the world. Diacetylmorphine, better known as heroin, was once introduced as a medicine; it was sold over the counter by pharmaceutical giant Bayer starting in 1895. Despite being originally advertised as a nonaddictive alternative to morphine, the true nature soon became known, leading to the Harrison Narcotics Tax Act of 1914 and the eventual banning of the drug in 1924.
It’s clear that drug manufacturers, doctors and politicians knew about the dangers of opiates over 100 years ago, but that didn’t stop a wave of opiate medications from hitting the market in the late 1980s and early 1990s. Manufacturers insisted that these medications were safe and complication-free, going so far as to promote studies backing these claims. Believing the research, doctors began to prescribe opiates to patients in pain, over and over and over.
Despite the marketing campaigns pushed by pharmaceutical companies, the truth has been revealed and the stats don’t lie: Prescription painkillers are every bit as addictive as heroin. Unfortunately, the damage is done. Decades of overprescription have contributed strongly to the current opioid epidemic, and without changing the very tenets of how doctors are educated, there is no change on the horizon.
In response to this long-lasting trend, state legislatures across the country are now cracking down. Doctors in many areas are now limited in how, when and to whom they can prescribe pain meds. While this is good news in terms of reducing the supply of opiates in circulation, it’s bad news for those who need access to reliable pain management.
Evaluating and Treating Pain in Patients
 Unfortunately, unlike most other metrics used to evaluate patient wellness, there is no objective way to measure pain, the location of pain or the source of pain when no physical cause is in play. Further, many people feel pain in radically different ways. Those with a high pain tolerance may find a deep gash, for example, to be simply irritating, while an individual with a low pain tolerance may be writhing in agony in response to the same injury. Accordingly, this opens the door to unclear methods of evaluation and no control to determine the relative pain of a particular set of circumstances.
Unfortunately, unlike most other metrics used to evaluate patient wellness, there is no objective way to measure pain, the location of pain or the source of pain when no physical cause is in play. Further, many people feel pain in radically different ways. Those with a high pain tolerance may find a deep gash, for example, to be simply irritating, while an individual with a low pain tolerance may be writhing in agony in response to the same injury. Accordingly, this opens the door to unclear methods of evaluation and no control to determine the relative pain of a particular set of circumstances.
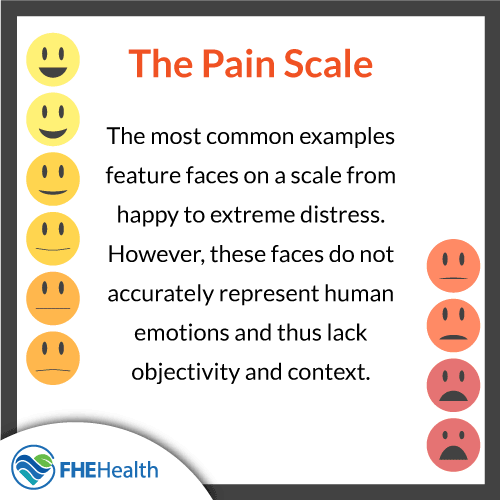
Often pushed by the need for hospital metrics, pain charts have become a common tool in an attempt to gauge patient pain. The most common examples feature faces on a scale from happy to extreme distress. However, these faces do not accurately represent human emotions and thus lack objectivity and context. Alternatives use a 1 to 10 pain scale, but asking patients to rate pain on a sliding scale is equally problematic, as context is important and many patients struggle to put pain in perspective in the moment. As such, many doctors and nurses fear doubting a patient’s opinions on pain, leading to a tendency to provide pain pills without stringent oversight.
This has led to an upsetting reality: Pain may be considered the fifth vital sign, but opportunities for evaluation are poor and common treatment avenues are proven to be dangerous.
Challenges Facing Pain Management
 One of the largest issues in appropriately addressing pain involves the presence of drug-seekers. These individuals come to hospitals, doctor’s offices, walk-in clinics and urgent care facilities claiming severe pain. However, this pain is not real; these patients are instead putting on an act for the sake of receiving prescription-only pain pills to feed an addiction. While experienced doctors and nurses can often identify pill-seeking patients, many of these individuals still slide through the cracks, contributing to the challenges in overprescription.
One of the largest issues in appropriately addressing pain involves the presence of drug-seekers. These individuals come to hospitals, doctor’s offices, walk-in clinics and urgent care facilities claiming severe pain. However, this pain is not real; these patients are instead putting on an act for the sake of receiving prescription-only pain pills to feed an addiction. While experienced doctors and nurses can often identify pill-seeking patients, many of these individuals still slide through the cracks, contributing to the challenges in overprescription.
The presence of these sorts of pseudo-patients is extremely damaging for those who do legitimately require pain medication or other alternatives to address acute or chronic pain. Yet, their reliance on pain medication may have been originally created from lax medication control. In identifying and treating pain, many doctors find themselves between a rock and a hard place — is a patient telling the truth, or are they lying to fuel their own addiction? Being forced to face these questions further negates the usefulness of pain as a fifth vital sign.
Taking Strides Toward Proper Pain Treatment
Doctors are working to improve pain management, including circumstances and prognoses to improve pain management outcomes, but there’s no easy way to solve the problem of objectively evaluating and addressing pain. However, this doesn’t mean others paths aren’t available. In innovative pain clinics, doctors are employing alternative techniques and treatments like:
- Acupuncture
- Medical marijuana, where legal
- Exercise, when physically possible
- Chiropractic manipulation
- Yoga
- Hypnosis
- Meditation
- Massage
- Biofeedback
Addressing an Addiction to Prescription Painkillers
Regardless of the reasons behind the use of pain medication, legitimate or not, addiction is always a possibility. Some people who began using pain medications for a true reason, and particularly those who are still experiencing pain, feel as though getting help isn’t an option. And, as the use of pain pills is so common, many people feel as though it’s not actually an issue. The reality, of course, is completely the opposite. It is possible to recover from an addiction to painkillers, even for those with ongoing complications in need of relief.






