Suicide can affect males and females of all ages. However, the Centers for Disease Control and Prevention (CDC) indicates the second leading cause of death among people aged 10 to 14 and 20 to 34 was suicide in 2021. Between 2000 and 2021, suicide rates increased by an alarming 36%. This article provides an overview of suicide rates by state and can help you understand factors influencing suicide, socioeconomic contributions to regional disparities and prevention efforts.
Understanding Suicide Rates
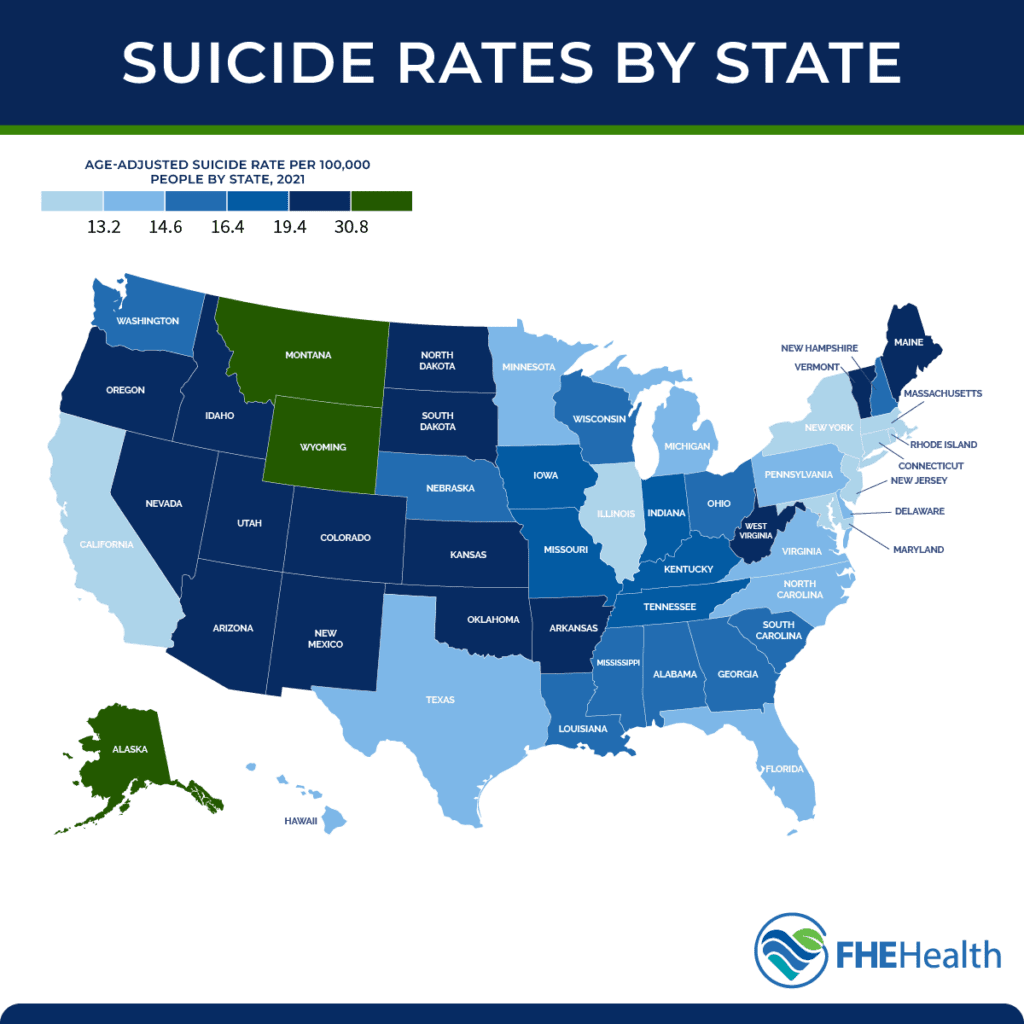
The CDC analyzes the number of people who die by suicide per 100,000 people within the total population of a given area to provide a rate per capita. It uses age-adjusted rates to compare differences within the population’s age distributions and changes within the population over time.
Besides age, other demographics are utilized to further understand suicide rates and populations potentially at higher risk. Demographic variables include gender, race and ethnicity, education level, employment status, geographic location and other factors that could influence suicide rates. Substance abuse, social isolation and mental health care access also help identify high-risk groups and regions.
By researching comprehensive data, communities can create policies and foster support to help reduce suicide incidences.
Factors Influencing Suicide Rates
There isn’t a single, isolated cause for suicide. Instead, several factors can influence suicide rates, including socioeconomic status, mental health conditions and access to health care.
Economic hardship and unemployment can increase stress and feelings of hopelessness, leading to higher suicide rates. Mental health disorders, such as depression and anxiety, are significant risk factors. Access to mental health services plays a critical role in prevention, with limited access often associated with higher suicide rates.
Social factors, including isolation, relationship issues and lack of community support, are also contributing components. Additionally, cultural attitudes toward mental health and suicide can influence the likelihood of a person seeking help. Understanding these factors is essential to effective suicide prevention efforts.
Analyzing Trends and Suicide Rates by State
Suicide rates by state vary due to many factors, including the availability of firearms, which are involved in more than half of suicides per KFF research. Other factors impacting state suicide trends include demographics, mental health status and access to mental health services. KFF research concluded that some of the highest suicide rates in 2021 were among people living in rural areas, where mental health services might be lacking.
According to suicide mortality data from the CDC, Montana had the highest death rate per capita at 28.7, while New Jersey had the lowest at 7.7. Looking at how firearm availability might have factored into these results, KFF’s research indicated Montana’s rate of suicide by firearm was 15.8, with the rate of other suicides at 10.2. In comparison, New Jersey’s suicide by firearm rate was 1.8, with other suicides at 5.3. Montana had only four firearm law provisions that year, while New Jersey had 80.
Regional Disparities and Socioeconomic Factors
Socioeconomic factors that can contribute to regional disparities in suicide rates include unemployment, income equality and access to education and health care. For example, regions with high poverty levels and joblessness often result in more people experiencing increased stress and mental health challenges.
These same regions may have limited access to quality health care and mental health services, making it challenging for people to get the help they need. Without access to appropriate services, issues worsen and may lead to higher suicide rates.
The ability to access higher education has been noted to decrease suicide risk. Education level may directly link to joblessness, as less education may result in fewer job opportunities. Lack of employment impacts socioeconomic status, further contributing to risk factors.
These and other disparities highlight the need for targeted interventions and resources to support vulnerable communities and reduce suicide rates.
Identifying High-Risk Groups and Vulnerable Populations
Based on the data from previously cited sources, an array of high-risk groups and vulnerable populations exist. Within age groups, adolescents and young adults are often included in high-risk populations. Younger people frequently face significant academic and social pressures that can increase the likelihood of suicidal thoughts. However, older adults can also be at higher risk, particularly those with chronic illnesses, those who’ve lost a loved one and those who face isolation.
Veterans and military personnel who’ve experienced stress and trauma during service could experience higher suicide rates. Likewise, individuals who’ve experienced a history of trauma or abuse may be more likely to consider or attempt suicide.
Individuals with mental health disorders may face significant stigma within their community, making them more vulnerable. LGBTQ+ individuals may also deal with discrimination and lack of support, increasing their risk. Social stigma and discrimination against any population for any reason could place them at a higher risk for suicide.
Intervention and Prevention Efforts
Despite the alarming rates, suicide is preventable through a comprehensive approach. The CDC lists numerous suicide prevention efforts in its Suicide Prevention Resource for Action. Strategies include:
- Fostering protective environments
- Identifying and supporting people at risk
- Enhancing access to and delivery of suicide care
- Reducing harms and preventing future risk
- Encouraging healthy connections
- Bolstering economic supports
- Teaching coping and problem-solving skills
Preventing future risk includes intervening after a suicide attempt. While communities should prioritize suicide prevention efforts to include activities most likely to reduce suicides, everyone can play a role in saving lives by learning the warning signs and committing to social change.
Reach Out for Help
Warning signs in others may include significant changes in behavior, especially after a loss or other painful event. When people use phrases relating to being a burden, having no reason to live or even coming right out and talking about killing themselves, they shouldn’t be ignored.
If you’re in crisis or emotional distress and contemplating suicide, don’t be afraid to reach out for help immediately. Contact FHE Health to talk with one of our compassionate counselors. We’re available 24-7 to ensure you have access to the help you need when you need it.