This article has been reviewed for accuracy by our peer review team which includes clinicians and medical professionals. Learn more about our peer review process.
Roughly one in ten Americans take an antidepressant, according to Harvard Health. In fact, antidepressants are the third-most common medications prescribed to people in the U.S.
Selective serotonin reuptake inhibitors (SSRIs) are a popularly prescribed type of antidepressant drug. Although these drugs may not cure depression, they can reduce the condition’s symptoms, including suicidal thoughts.
condition’s symptoms, including suicidal thoughts.
SSRIs are a class of drugs that encourage the brain to produce more serotonin, making them effective in treating mental health conditions such as depression and anxiety. While many people choose to stay on this medication for an extended period, some choose to end treatment due to side effects or because they want to transition to medication-free alternatives. In this article, we cover information on the recovery time of SSRI treatment and factors that may affect it.
Understanding SSRIs and Recovery
Currently, research indicates that there’s minimal risk associated with staying on SSRIs long-term. Before starting on this drug therapy, it’s helpful to understand how SSRIs work and what to expect from treatment.
What are SSRIs?
SSRIs are a popularly prescribed type of antidepressant drug that tend to be effective in reducing depression, anxiety, PTSD, and other mood disorders without many side effects. Common types of SSRIs include citalopram (Celexa), paroxetine (Paxil), sertraline (Zoloft) and escitalopram (Lexapro).
This class of medications works by increasing levels of serotonin in the brain. Serotonin is a chemical messenger that carries signals between nerve cells and the brain, regulating mood, sleep, behavior and memory and playing a key role in well-being and happiness. Along with causing the brain and body to produce more serotonin, SSRIs block the brain cells from absorbing serotonin after it’s performed its function. This means that more serotonin is available to pass messages to the brain, prolonging its benefits for mood management. This makes SSRIs an effective option for treating symptoms of depression.
Typical Duration of SSRI Treatment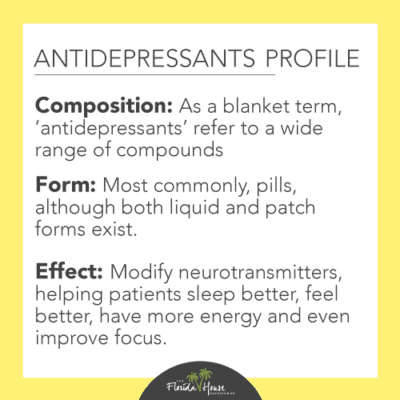
SSRIs are usually a physician’s first choice when treating someone with persistent or even severe depression because they are associated with a high degree of efficacy and are generally safe with few side effects. They’re often used in conjunction with cognitive behavioral therapy (CBT).
How long an individual stays on an SSRI depends on a variety of factors, such as how effectively the medication controls their symptoms, whether they experience bothersome side effects, and whether they’re at risk of complications from the medication. Most doctors recommend their patients stay on the medication for four to nine months before deciding to go off of it. According to information from the National Center for Health Statistics, about two-thirds of Americans taking SSRIs have been on their medication for at least two years, and a quarter of people have been on them for more than a decade.
Recovery Timeline from SSRIs
Going off SSRIs without tapering off of them under the direction of a psychiatrist can cause antidepressant withdrawal symptoms. Unlike withdrawal from a narcotic or powerfully addictive drug, these withdrawal symptoms aren’t regarded as medically dangerous, but they can be downright uncomfortable. They occur because the brain’s neurons haven’t had the chance to adapt to the suddenly reduced level of neurotransmitters. About 56 percent of SSRI users experience withdrawal symptoms, with about 46 percent of people reporting severe symptoms.
Immediate Post-Treatment Phase
Symptoms of withdrawal typically begin during the first few days after the individual stops taking the antidepressant and peak between the first and second weeks. During the first weeks of discontinuation, individuals may experience headaches or increased irritability. Other symptoms can include nausea, insomnia, tiredness, and/or anxiety. In severe cases, a person might experience a range of flu-like symptoms that include chills and achiness.
Short-Term Recovery (1-3 Months)
After peaking, symptoms tend to decrease in severity, though they can still be bothersome. Individuals may continue to experience changes in their mood and energy levels, and they may experience headaches and bouts of nausea.
In some cases, SSRI withdrawal can look like depression. However, several signs can indicate that the individual is experiencing withdrawal, not a relapse of depression. For example, if symptoms emerge quickly after stopping the medication but subside when the individual takes a dose of medication, they’re likely due to withdrawal. Additionally, if the individual experiences physical symptoms not common with depression, it’s likely the result of stopping treatment. On the other hand, if symptoms persist past the first month and continue to worsen, it may be a relapse.
Several factors influence how an individual experiences SSRI withdrawal. Newer research indicates that the longer someone took the medication, the more difficulty they experience when going off it. Additionally, the higher the dose they were on, the more intense their withdrawal symptoms tend to be.
Long-Term Recovery (3-12 Months)
In the months following SSRI cessation, side effects tend to taper offer considerably, with the majority of people seeing them go away entirely. However, the duration of withdrawal symptoms varies widely, with some patients reporting problems as long as 79 weeks after stopping treatment.
Managing the Recovery Process
As you’re recovering from SSRI treatment, it’s important to find support and practice self-care. While the withdrawal process doesn’t pose a direct threat to your health, it can impact how you feel physically and emotionally. Particularly if you have a history of depression, you may need to closely monitor your symptoms and stay in touch with your healthcare provider.
Professional Guidance
Healthcare providers typically recommend that patients not quit using SSRIs, like sertraline and cold turkey. In most cases, doctors encourage patients to taper off SSRIs with diminishing doses. Patients, in consultation with their doctor, should carefully consider their history of depression and if stopping the use of these medications is in their best interest. Throughout the withdrawal process, it’s important to keep your doctor’s appointments so that your healthcare provider can monitor your symptoms and help you manage them.
Statistically, while 20% of U.S. adults have received mental health treatment in a given year, only about one in 10 have received counseling from a mental health care professional. If you aren’t currently seeing one, it may be a good idea to connect with a therapist as you navigate the SSRI withdrawal process.
Self-Care Strategies
As your body is going through withdrawal, it’s important to practice self-care by making healthy lifestyle choices and finding effective stress management techniques. This includes:
- Following a healthy, balanced diet: What you eat is an important component of mental health. Current guidelines recommend a high intake of fruit, vegetables, whole grains, fish, low-fat dairy and healthy fats for those managing mental illnesses such as depression.
- Keeping a regular sleep schedule: Getting adequate sleep can help you manage withdrawal symptoms by supporting healthy brain functioning. It can also help to prevent relapses of depression.
- Stay active: An active lifestyle with regular exercise goes a long way in helping you manage stress. Additionally, it boosts your brain’s serotonin levels, which can offset changes in these levels as you taper off SSRIs.
- Find a support system: Your healthcare provider, therapist, friends and trusted family members can provide invaluable support as your body comes off of medication. If people around you are aware that you’re ending SSRI treatment, they’ll be less likely to take mood changes personally.
Tapering Off of SSRIs: Other Things to Know

Patients, in consultation with their doctor, should carefully consider their history of depression and if stopping the use of these medications is in their best interest.
Doctors can guide patients through this decision-making process. Some people may wish to go off antidepressants after six months to a year, but doctors recommend that patients who have had more than three recurrences of depression remain on SSRIs or another antidepressant for at least two years.
Clinicians are not likely to recommend going off antidepressants during major life changes or during stressful events like divorce or illness. Ideally, patients should feel stable and confident that they are functioning well before tapering off their medication. Patients who do decide to stop using SSRIs should discuss a tapering plan with their doctor. Most clinicians will recommend reducing the medication dose incrementally, often with a space of six weeks between reductions. This schedule can vary in accordance with the current dose a patient is taking, the type of SSRI in question, and the length of time they’ve been taking the medication.
Clinicians are also likely to encourage patients to keep track of their moods and report any serious mood disturbances. They will also recommend that patients take self-support seriously. Counseling, exercise, and reliance on a support system can help people maintain their mental health and keep depressive symptoms in check. In fact, it’s been shown that people who exercise at least three times a week are less likely to experience a recurrence of their depression.
“How Long Does Sertraline Withdrawal Last?”
Many people want to know how long withdrawal is for certain SSRIs in particular, such as sertraline (Zoloft). With any SSRI, not just sertraline, the length of time can vary from person to person. These withdrawal symptoms will improve with time, but they can be unpleasant for days and possibly even weeks. In time, the brain returns to a normal state after stopping antidepressants. If depressive symptoms do arise and gradually worsen, it’s best to consult a psychiatrist or doctor if they don’t improve within a few weeks or if they become severe.
Healthcare providers typically recommend that patients not quit using SSRIs cold turkey. In most cases, doctors encourage patients to taper off SSRIs with diminishing doses. Most clinicians will recommend reducing the medication dose incrementally, often with a space of six weeks between reductions. This schedule can vary in accordance with the current dose a patient is taking, the type of SSRI in question, and the length of time they’ve been taking the medication.
SSRIs Popularity: “Safe and Effective” for Depression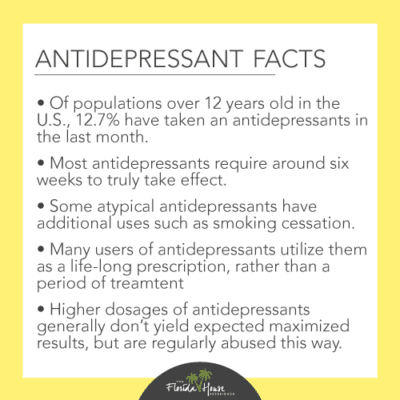
In recent decades, the use of antidepressants has increased by as much as 400 percent. SSRIs are usually a physician’s first choice when treating someone with persistent or even severe depression because they are associated with a high degree of efficacy and are generally safe with few side effects. They’re often used in conjunction with cognitive behavioral therapy (CBT).
Before the development of SSRIs, the pharmaceutical realm had few drugs to treat mood disorders such as depression and general anxiety. Then fluoxetine, better known to the world by the brand name “Prozac,” gained FDA approval in 1987. The medication revolutionized the treatment of depression and paved the way for the development of other SSRIs with fewer side effects.
Prozac also helped to bring the problem of depression out into the open. People grew less hesitant to talk about their depression and to seek treatment. (Of course, Prozac is not without some side effects. Pharmaceutical companies have continued to refine and produce SSRIs with fewer side effects.)
Are There Risks of Combining SSRIs Like Sertraline and Other Drugs?
Combining SSRIs like sertraline with other drugs or alcohol can pose risks and is generally not recommended. Alcohol can increase the nervous system side effects of sertraline, such as dizziness, drowsiness, and difficulty concentrating, can lead to risk of cancer, and can also exacerbate the depressive symptoms that sertraline is intended to treat. When it comes to other drugs, sertraline can interact negatively with a wide range of medications, leading to increased side effects or decreased effectiveness. For instance, combining sertraline with other drugs that increase serotonin — such as certain antidepressants, pain medications, or herbal supplements like St. John’s wort — can lead to a potentially life-threatening condition called serotonin syndrome. This condition can cause symptoms like agitation, hallucinations, rapid heartbeat, fever, muscle stiffness or twitching, and nausea. Always consult with a healthcare provider before combining sertraline with any other substances.
What Are the Effects of SSRIs?
The brain produces certain “feel-good” chemicals—among them, the neurotransmitter serotonin. Serotonin is associated with feelings of relaxation and calm. Typically, it is absorbed by the bloodstream after circulating in the brain. However, depending on the person, this process can leave the brain without enough serotonin to produce those feelings of relaxation and calm. SSRIs facilitate the reuptake of serotonin in the brain so that more of it is available.
Researchers are not entirely sure what about this feature of SSRIs makes them therapeutic for depression. One theory is that depressive disorders are associated with lower levels of serotonin and dopamine in the brain and that because SSRIs cause more serotonin to remain in circulation in the brain, they relieve depressive symptoms. In fact, many people report feeling completely back to normal when taking these medications.
Although SSRIs are similar in nature to one another, their side effects and tolerability can vary from one person to the next. Similarly, the dosage can differ markedly between individuals as well.
While generally speaking, there are fewer side effects associated with these drugs, there can be effects aside from the reduction in depressive symptoms. First, SSRIs don’t work optimally for people in every case. Some people do not experience relief from their depression and may require different types of antidepressants or even a combination of them to experience relief.
Some common side effects of SSRIs include:
- Headache
- Drowsiness or fatigue
- Dry mouth
- Nausea
- Weight gain
- Sexual dysfunction
For some people, these side effects will diminish over time. Others may find them intolerable. Physicians may replace an SSRI with another if one is causing too many unpleasant side effects. A change in prescription sometimes helps.
One question that often pops up in conjunction with these drugs is: How long should an individual take them? Answers vary. Patients who experience circumstantial depression and have no prior history of clinical depression may eventually choose to discontinue their use of SSRIs, like sertraline, after a year. On the other hand, people who have habitual depression may choose to take these drugs indefinitely to guard against severe depressive episodes.
When to Seek Help
If your SSRI withdrawal symptoms are still bothersome after several weeks, or if you experience a return of depression symptoms, it may be time to seek help from a mental health provider. A therapist may recommend a short course of medications such as antihistamines, anti-anxiety medications or sleep aids to help you navigate the recovery process. They can also help you track depression symptoms and recommend treatment options if you experience a relapse. 
FHE Health specializes in mental health treatment as well as substance addiction therapy. Our clinicians have the expertise to treat patients with all types of mood disorders, including anxiety and depression. SSRIs are an important drug in the arsenal of treatments for mental illness. Our psychiatrist and medical team prescribe them and also routinely help patients taper off of these drugs.
It’s important for patients to remember that each individual, their brain chemistry, and their circumstances are different. Some people may need to rely on SSRIs for a longer period of time or indefinitely. Others will be able to safely and smartly taper off an SSRI with the help of our doctors.
Conclusion
For most people who come off of SSRIs, withdrawal symptoms peak between one and two weeks, then gradually taper off as the body returns to normal functioning. In rare cases, individuals may experience withdrawal symptoms months later. Fortunately, finding support and practicing self-care can help you navigate this challenging phase more effectively.
Remember, you’re not alone in your mental health journey. Reaching out to friends, family and mental health care professionals can provide encouragement and understanding as you find other ways to manage your mental health.
Got a question? We’re here to help. Contact us anytime.