
Post Traumatic Stress Disorder, better known as PTSD, is a common mental disorder affecting around 8% of the population at any given time. PTSD is the result of witnessing or experiencing a stressful experience, such as fighting in a war, physical or sexual assault, surviving a natural disaster, or anything else that results in fear, acute stress or anxiety. The condition can be debilitating when symptoms are at their peak.
PTSD can have many causes, and different people will respond in varying ways to the same events. Something like escaping from a building fire may not leave a lasting mark on one person but may cause signs of PTSD in another. Regardless of the cause, however, symptoms tend to be more alike than different. One of the most notable symptoms for a majority of those affected by PTSD is self-isolation.
Need Help?
Treatment can begin quickly and discreetly, get started now
What Is Self-Isolation?
Self-isolation refers to the tendency to separate oneself from others. Rather than going to parties, taking part in team events, hanging out with friends or spending time with family members, individuals will instead choose to spend time alone.
While it’s normal for everyone to crave solo time on occasion, self-isolation goes far beyond forgoing a few events. Those who self-isolate completely retreat into themselves, allowing the stress involved in seeing others and taking part in normal activities to prevent participation in previously pleasurable behaviors.
Self-isolation can be a symptom of other forms of mental illness, like depression or anxiety disorders, but it is a key side effect of PTSD. PTSD and isolation often go hand-in-hand.
Start Treatment Now
Treatment can begin quickly and discretely, get started now
Why Do Individuals with PTSD Socially Withdraw?
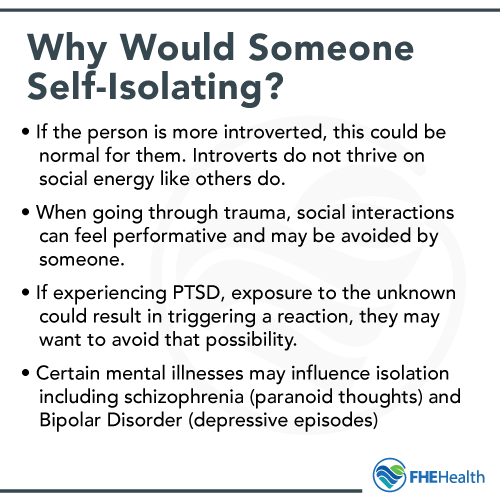
In many ways, self-isolation is a form of self-preservation. When one is alone and not in the presence of other people, whether friends and family or the general public, the chance of triggering events feels much less likely. Traumatic events like seeing people die, facing abuse or getting into a fight probably won’t occur when staying isolated and alone.
Self-isolation is also the result of feeling alone, abandoned and misunderstood. Those with PTSD are often acutely aware of the fact that the experiences that led to post-traumatic stress are unique to them, and even those who may have been present won’t necessarily understand the response. By isolating themselves, PTSD sufferers can avoid negative responses or continued efforts to explain feelings.
PTSD-induced social withdrawal may not be a conscious choice. As individuals struggle to deal with their feelings, being alone seems like the easiest option.
PTSD and Isolation in Veterans
Veterans are among the most likely to develop PTSD and, unfortunately, are at the highest risk for serious side effects. Self-isolation is extremely common after returning from a war zone; men and women who return home will push friends, family and even their spouses away, ruining relationships and exacerbating the issue.
Being around other people after coming out of the service can be overwhelming and uncomfortable without PTSD, but those who have seen awful things while deployed will have a more difficult time in a way that the average civilian can’t understand. This leads to even higher correlations between PTSD and isolation in these populations.
Begin your recovery today
Ready to start? More questions about treatment?
Why Trying to Reach Out Doesn’t Work
Reaching out is often the first instinct of those who are watching their loved ones go through PTSD and isolation. It’s not uncommon for friends and family to try to make an extra effort to plan events, stop by to visit or otherwise inspire more social behavior. However, this is unlikely to make a difference.
Those who are self-isolating will see efforts to change their behavior as further evidence that no one understands what they are going through. They may believe that their differences are now more pronounced than ever and that there is no hope for feeling happy or normal again. Those who are deep in isolation will likely rebuke all invitations, choosing instead to fall further into this troublesome behavior pattern.
Why is Self-Isolation Dangerous?
Self-isolation as a coping method may seem harmless, but this is generally not the case.
First, those who self-isolate often find themselves consumed by their challenges rather than working to find the strength to get help. As isolation accelerates, encouraging getting therapy or medical treatment for PTSD will become far more difficult. As such, taking action early is often the best way to get in front of this symptom of PTSD.
In extreme cases, isolation may pose a threat to physical health and wellness. Isolation can lead to depression, which in turn can lead to troubles at work and job loss, financial problems, lack of self-care and failure to seek medical attention. Extreme cases may even entertain suicidal ideations that could, if left unaddressed, lead to action.
The Cycle of Isolation
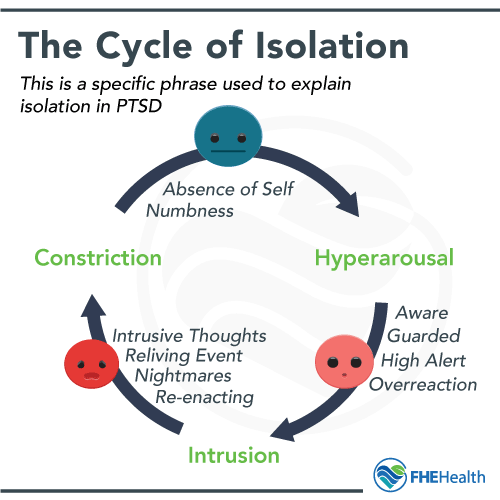
The cycle of isolation refers to how those with PTSD may isolate themselves in cycles depending on how they respond to these three stages: hyperarousal, intrusion and constriction.
In the hyperarousal stage, individuals are very guarded and on high alert, and they may be likely to lash out with aggression. During the intrusive thoughts stage, it’s common to relive traumatic events in conjunction with graphic nightmares.
The constriction phase results in numbness and an absence of self. This is the stage most commonly associated with self-isolation, even though this can happen at any given time throughout the cycle. However, manifestation can differ significantly from one individual to another, and reactions can vary greatly, even among those who have endured similar experiences.
The cycle of isolation is important for friends and family concerned about a PTSD-affected individual to understand. As this kind of behavior can move in circles, a decrease in isolating behaviors may not mean the individual is in a better state of mind. As such, getting help should still be encouraged, even when trends appear to improve on the surface.
How Can I Help Someone with PTSD Social Withdrawal?
Someone you care about pulling away from the world because of PTSD can be tough to watch. Knowing what to do or say isn’t always easy, but your support matters more than you might realize. So, how can you help someone suffering from PTSD and isolation?
Acknowledge what you don’t know first. Their experience isn’t yours, and that’s okay. What matters is reminding them they don’t have to face it alone. Let them know you care, you see them, and help exists. Sometimes, making plans with no pressure, sending a message, or checking in makes all the difference.
Options are out there—recovery groups, treatment centers, therapists. Offering is enough; pushing isn’t necessary. Believing help is worthwhile can be enough to plant the idea.
FHE Health offers outpatient and inpatient PTSD treatment. We’re here to help if you need options.
More Questions about Treatment?
We offer 100% confidential and individualized treatment
About Chris Foy
Chris Foy is a content manager and webmaster for FHE Health with years of experience in the addiction treatment industry...read more









