
A psychotic break can happen suddenly but with the potential to cause lifelong issues. Learn what a psychotic break is, as well as the symptoms, triggers and treatments, so you can seek help appropriately or recognize risk factors or psychotic episodes your loved ones may be experiencing.
What Is a Psychotic Break?

A psychotic break is what happens when a person’s mind loses its grip on situations experienced or the reality they’re surrounded by. According to the psychotic break definition accepted by the medical community, during an episode of psychosis, you may begin to experience hallucinations. Although someone observing or treating you will realize your experience isn’t grounded in reality, you may not be able to discern that.
After the episode, you may remember part or all of the hallucination as actually occurring instead of being the product of your mind. Additionally, you may be under the control of delusional beliefs during a psychotic episode. If you’re able to discern that you’re in the midst of a psychotic episode, you may feel frightened or angry. This can cause you to strike out at anyone who’s with you at the time. If alone, the hallucinations or delusions may cause or convince you to harm yourself.
The symptoms you exhibit may cause you to wonder if you’re experiencing a psychotic break rather than a nervous breakdown. During the psychotic episode, however, you may believe your experience is real. This can lead you to deny that you’ve had any type of psychotic break. If you’re worried you may be exhibiting symptoms of psychosis or wonder exactly what a psychotic break is, it’s important to reach out to a mental health professional or a trusted loved one to begin the process of obtaining treatment.
Spotting the Signs of Psychosis
Spotting the signs of psychosis may be difficult for those in the midst of a psychotic break. Family members, friends and coworkers may be the first to observe psychotic symptoms during an episode. When that occurs, the person experiencing psychosis may not believe they have a problem when their loved ones express concern or recommend seeking help.
Signs of psychotic break can include:
- Hallucinating. Seeing people, places or objects that don’t exist in reality or can’t exist in the manner in which they’re seen. Hallucinations can also include auditory experiences — hearing people that aren’t currently with you or incidents that aren’t occurring.
- Delusions. Succumbing to beliefs not grounded in reality. Delusions may present in confusingly opposite ways, ranging from becoming suspicious of everyday occurrences or people you normally trust to believing you’re something you aren’t or have powers you don’t actually possess.
- Disordered reasoning. Talking about or acting and thinking in a disorganized manner. This includes jumping between thoughts that are unrelated, equating beliefs that are actually divergent or making little to no sense in what you share with others verbally or in written form.
- Extreme anxiety. Becoming enormously worried over situations that don’t exist in reality or because of unreasonable fear and suspicion of others. This can lead to an inability to concentrate due to experiencing obsessive beliefs that distract from normal life activities.
- Catatonia. Being in a state of unresponsiveness. This may be the result of your body’s instinct to protect itself from dangerous thoughts and actions during an episode or be triggered independently as your psychosis deepens.

What Triggers Psychosis?
Psychosis can be triggered by many different medical and mental health conditions, as well as occurrences in everyday life.
Mental health psychosis triggers may include:
- Schizophrenia. This disease makes it hard for patients to discern reality from unreality. Patients diagnosed with schizophrenia may advance beyond this lack of discernment to experiencing a psychotic episode where those beliefs deepen or are acted upon.
- Bipolar disorder. During the manic phase of bipolar disorder, reality can slip away from the patient, and the resulting psychotic break can lead to dangerous behaviors common during mania. Psychotic episodes may also occur during the depressive phase as thoughts darken rapidly and lead to beliefs not rooted in reality.
Physical health issues that may lead to psychosis include:
- Dementia
- Drug and alcohol abuse, leading to meth psychosis or alcoholic psychosis
- Diseases and disorders like HIV/AIDS, brain tumors, strokes, epilepsy, Parkinson’s and Huntington’s
Common triggers of psychosis also include trauma and extreme stress.
Who Is at Risk for Psychosis?
Anybody, despite or because of their life experiences and genetics, can experience a psychotic break or ongoing psychosis. However, people whose close family members have a psychotic disorder may have an increased risk of developing one themselves. Additional risk factors include people who have the 22q11.2 genetic mutation, which can lead to psychosis and schizophrenia. Patients diagnosed with disorders affecting the brain may also have an increased risk of having a psychotic break.
If you believe you may be at risk for psychosis, you may actually be in danger of believing yourself psychotic when you are not. Only a small subset of people who have genetic or other risk factors actually develop psychosis. If you believe this outcome to be inevitable, however, you may create a self-fulfilling prophecy of experiencing psychosis yourself. Speaking with a qualified healthcare professional can help you see the difference between a risk of psychosis and actual experience of psychosis. Only three people out of every hundred will experience a form of psychosis within their lifetime, with about 100,000 people suffering their first psychotic episode each year.
What Does Psychosis Look Like from the Outside?
From the accounts of individuals who’ve gone through psychotic episodes and received treatment for psychosis, the primary presenting element has been confusion. The person looks, acts and sounds confused. Nothing they do or say seems connected to reality, even though they appear to be trying desperately to make sense of what’s going on around them. People with psychosis may talk to themselves, look fearful and bewildered, be totally out of touch with reality or begin speaking about subjects they have no knowledge or expertise about.
It’s vital for bystanders and observers to realize that someone in the midst of a psychotic episode is probably scared. Nothing makes sense to them, and this out-of-control feeling has them reeling.
How Long Does a Psychotic Episode Last?
A psychotic episode may last for 30 days or less. This type of psychotic episode is called a brief psychotic disorder and may only occur once. This is often true of drug-induced psychosis that results from the chronic use of certain drugs, such as opiates, methamphetamine, marijuana and alcohol.
But the psychotic episode may also last 6 months or even longer and repeat itself. Psychotic episodes that are a symptom of schizophrenia fall into this category. Someone with diagnosed (or undiagnosed) bipolar disorder can experience a psychotic episode during the manic phase of the disorder, which can persist for weeks to months.
What Are the Two Significant Signs of Psychosis?
While there are many signs of psychosis, delusions and hallucinations stand out as the most significant. These often occur during the acute phase of psychosis.
What Are Delusions?
Delusions refer to beliefs that aren’t based on reality. When someone is in psychosis, they may believe others are out to get them out of spite or vengeance or because of irrational hatred or dislike of them. When delusional, the individual likely doesn’t trust even those they generally trust implicitly, such as loved ones and family members.
A delusional individual in the middle of a psychotic episode may believe they possess supernatural or superhuman powers, have extraordinary insights or can foretell the future. This belief is entirely irrational and divorced from reality. When in psychosis, for example, a person may believe they can leap from a tall building and fly or perform other incredible feats that defy the limits of human powers, strengths and capabilities. (When someone’s beliefs are sufficiently divergent from reality, a diagnosis of delusion disorder may be appropriate.)
What Are Hallucinations?
Someone who’s hallucinating may see and hear people who aren’t there or places and surroundings that aren’t physically present. The person may see things in multiple ways, none of which may be remotely possible. For example, during a psychotic episode, a person may see and hear or interact with individuals in a historical event, like participating in the Olympic Games, rescuing people trapped in a burning building, ascending the throne of a magical kingdom and other far-fetched scenarios.
Some hallucinations are auditory replays of conversations with real or imaginary companions, strangers or loved ones. These conversations may have occurred, or they may not. The individual experiencing the hallucination believes they’re real when they aren’t.
What Does Being in Psychosis Feel Like?
Anecdotal accounts of individuals with psychosis express a common theme about what a psychotic break is experienced as: feeling confused about themselves and their surroundings. Many individuals also become upset with others they interact with, even family, close friends, coworkers and neighbors. There’s a strong sense of being out of control, and someone in a psychotic episode is likely to lash out at others in wildly unpredictable ways. They may even act in a threatening and violent manner in a desperate attempt to control what’s become uncontrollable in their lives.
Often, however, psychosis means the person is in greater danger of harming themselves than anyone else. Never ignore self-harm behaviors and indications of intent to hurt themselves. Loved ones and family members should watch for signs of self-harm behaviors or intent, especially if such acts continue or escalate. Get help for the individual promptly if such symptoms are present.
Can Drugs Cause Psychosis?
Both illicit and prescription drugs may cause psychosis. This outcome is rare with doctor-prescribed drugs, but not unheard of, and is typically centered around stimulant medications and steroids. Prescriptions used illicitly and in very large doses may also cause psychosis, including antihistamines, antidepressants, anticonvulsants, pain medications and muscle relaxers. Street drugs, including cocaine and hallucinogens, can lead to psychotic breaks. Methamphetamines can lead to a particular psychotic disorder commonly referred to as meth psychosis, which can occur in up to 40% of addicts who use this drug.
How Is Psychosis Treated?
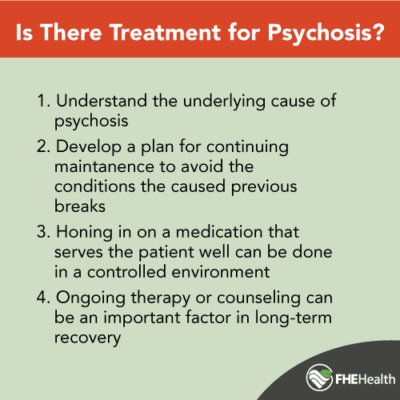
Psychosis relies on interrelated treatments that combine to address the acute phase of a psychotic break, as well as continuing maintenance of the symptoms and any underlying disorders. Antipsychotic drugs are typically the first line of treatment in cases of psychosis. This type of prescription response is customized for patients to address the schizophrenia, bipolar disorder or other mental health disease causing their psychosis. Other drugs in this class are best for treating specific psychotic episodes. Some commonly used medications include Seroquel, Risperdal, and Haldol. Complementary medications to address anxiety and depression may also be prescribed.
Successful psychosis treatments also include intense psychotherapy. Methodologies like cognitive behavior therapy (CBT) can be effective in the treatment of psychosis. Ongoing therapy or counseling can be an important keystone to recovery, particularly in the case of underlying disorders leading to psychosis. In the case of persistent or chronic psychosis, ongoing drug and clinical therapy should be pursued.
Seeking Help for Psychosis
If you believe you have experienced a psychotic break or fear a loved one may be affected by psychosis, seek help as soon as possible. Contact us at FHE today to reach our highly qualified cadre of counselors. Our hotline is available 24/7/365 to help patients begin the road to recovery right away.






