
Awareness of mental illness and the importance of treatment has been growing in recent years, thanks to numerous campaigns and celebrity efforts to raise awareness of conditions like addiction, depression, anxiety disorders, and self-destructive behaviors. Despite this progress, many Americans continue to go without help for treatable mental health conditions. And, all too often, those who are the most in need of treatment are the ones who are least likely to seek it out. According to the World Health Organization, in 2024, two-thirds of people living with mental health conditions don’t receive treatment around the world.
Addressing a Loved One’s Mental Health Needs
Much of the time, only a family intervention by family and close relatives addressing a loved one’s mental health needs will be the decisive factor that helps that person access help and a better quality of life. After all, just as someone with a severe case of influenza may not be able to drive themselves to their doctor’s office, someone with a severe mental health disorder may not be in a mental state that allows them to seek treatment on their own initiative.
Consider, for example, someone living with depression. The idea of finding a therapist and scheduling an appointment may feel like an impossible task. Similarly, social anxiety disorder can make it difficult to pick up the phone and make a call.
This is why the support of family and friends is so important to those living with a mental health disorder. With a mental illness intervention, the difficult first steps of identifying the problem, connecting with a qualified mental health care professional, and initiating the treatment process are already taken. For many people, this removes significant roadblocks to treatment and provides them with a clear successful and long term path to recovery.
Understanding Mental Health Interventions
Mental health interventions are not like addiction interventions. Because of the nature and complexity of mental illness, a different approach is necessary. While the goal of both types of interventions is to help the individual recognize that they need professional help managing a condition, a mental illness may not allow someone to see that they have a problem and help is needed, even when they’re presented with evidence.
A meeting with a large group of friends and family who discuss the negative impacts of their loved one’s addiction can be an eye-opening experience. However, someone living with a condition like depression or bipolar disorder is highly unlikely to react in the same way. A much smaller group of just one or two friends or family members will likely create an environment more conducive to success.
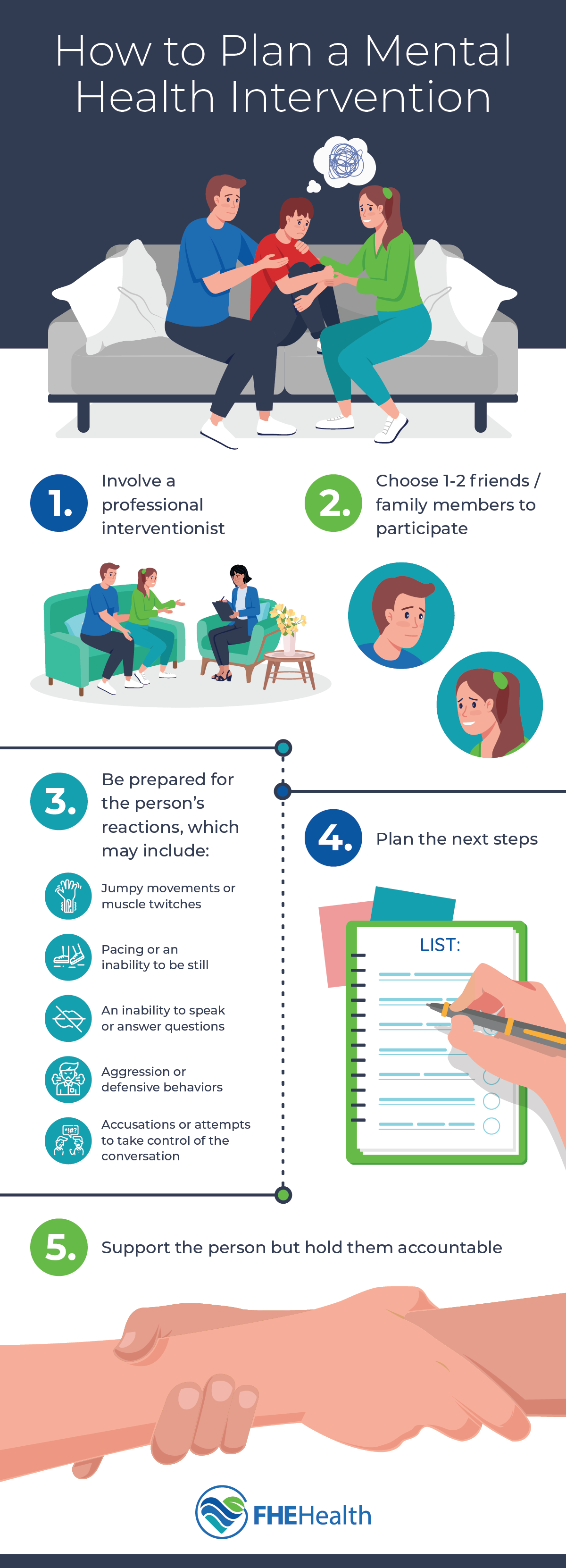
When someone’s behavior and reactions are heavily influenced by an untreated mental health disorder, unexpected and unpredictable behaviors may result. Depending on the nature of the disorder, they may exhibit:
- Jumpy movements or muscle twitches
- Pacing or an inability to be still
- An inability to speak or answer questions
- Aggression or defensive behaviors
- Accusations or attempts to take control of the conversation
In extreme cases, the person may even become violent. It’s important to have an experienced interventionist who is trained to deescalate behaviors and handle challenges as they arise.
Two Types of Mental Health Interventions
There are two main types of interventions for mental health, each of which requires a different approach.
Crisis Interventions
A crisis intervention is appropriate when the person is in the middle of an episode-type event. For example, this type of intervention is suitable when someone with schizophrenia is experiencing catatonic behavior or delusions.
Unlike an addiction intervention in which family and friends come together and tell their loved one how his or her addiction has affected them, having a group of people involved in a mental health crisis intervention is only likely to escalate the problem. Generally speaking, crisis interventions require teams of specially trained staff that are available 24 hours per day and specialize in quickly transitioning the client to intensive treatment in a community-based setting. This type of treatment aims to de-escalate the situation and prevent hospitalization.
Interventions for Worsening Conditions
Not all mental health conditions are marked by dramatic episodes of hallucinations or delusions. For most people with mental problems, the condition leads to emotional distress and problems with work, social, and family activities. This may present as decreased job performance, worsening communication with friends and family, or the inability to care for oneself. There’s also a wide spectrum for difficulty functioning: some people are high-functioning with depression and anxiety, and signs of their suffering are easy to miss, while other people struggle to get out of bed and fulfill obligations.
If a loved one is exhibiting warning signs like a loss of interest in activities they used to enjoy or profound changes in sleep patterns—especially if their ability to function is declining—then it may be time to stage a mental health intervention.
Mental illness is very complex, and the success of an intervention hinges on the involvement of a trained professional. In some cases, mental health illnesses have overlapping symptoms, and substance abuse issues can make signs of the illness difficult to recognize. The individual may also deny that they have a problem or that professional help would benefit them, or they may believe that they know what’s best for their health and they’re opposed to taking medication or meeting with a therapist. This is why mental health interventions must take place under the supervision of an experienced professional interventionist.
Planning a Mental Health Intervention
Interventions are go-to plot devices in countless movies, television shows, and books, making them a familiar concept to many. Unfortunately, too often, well-meaning friends and family members attempt to carry out interventions with minimal professional input and oversight. If a mental health intervention isn’t done correctly, the person can feel like they’re being attacked by people they trust and they can quickly become defensive.
The more preparation goes into the intervention, the greater the likelihood of success. Emotions can run high, so it’s best to prepare a script and stick to it. An interventionist helps strategize what participants can say if their loved one responds in a certain way. The most important thing is to set a positive, supportive tone. Ensure that the individual is treated with love and respect and maintain a calm, level tone, even if they react unpredictably.
Because many who live with mental illness feel trapped, it’s helpful to lay out a clearly defined plan with options for the individual to choose from. By making the process of getting help as effortless as possible, the person living with mental illness is more likely to pursue treatment.
A Note About Legal Mental Health Intervention
Involuntary commitment laws exist in all 50 states and the District of Columbia, though the specific criteria and procedures vary significantly by state. These laws permit the involuntary detainment and treatment of individuals with a mental illness or substance use disorder who are deemed a danger to themselves or others, or unable to care for their basic needs. An example, the Baker Act is a Florida law that allows families to provide emergency, involuntary mental health services and temporary detention for those who are impaired because of mental illness and are unable to recognize their need for treatment. For example, if someone is a danger to themselves or others, they could be committed to a psychiatric unit for up to 72 hours. This act can only be invoked by law enforcement, mental health professionals, physicians, and judges.
Important Tips for Planning a Mental Health Intervention
If you and/or your family are planning to stage a mental health intervention for a loved one, there are some tips/steps you might want to include in your plan. Use this list of ideas to support a successful intervention.
Be Mindful When Choosing Participants
Keep your intervention group to participants you know whom your loved one trusts. Avoid choosing individuals who are likely to go “off plan” and unlikely to behave in a calm manner or are likely to trigger your loved one. Even family members who love and care for one another don’t always get along. It may be best to include members of the family in your intervention who your loved one is comfortable with.
Have a Post-Intervention Plan
The goal of your intervention is to persuade your loved one to get into treatment. While their agreeing to treatment is a goal, too, the treatment is actually what’s crucial. Be sure that you have treatment lined up so that there’s a clear plan to follow once your loved one does agree to get help. Be sure you’ve contacted a mental health treatment center. Discuss insurance and all the other prerequisites involved in enrolling for treatment. Performing this legwork will make it easy for your loved one to go from intervention to treatment. Without a plan, your loved one might feel less inclined to seek help during the interval between intervention and treatment.
Convey Support
Let your loved one know that you intend to support them as they go through treatment. They’re likely to feel scared and overwhelmed. Reassure them that they won’t be alone as they enter treatment and follow a treatment regimen.
Be Discreet
Remember that your loved one’s mental health is their private business. By staging an intervention, you are shining light on their mental state, and that’s an action not to be taken lightly. Be sure that you limit discussion of the intervention to only participants. Your loved one may feel angry or threatened if they believe you’ve shared information about them beyond their inner circle. Ensure that the place you stage your intervention is also a discreet choice.
Consult with a Professional Intervention Specialist
It can be helpful to partner with an intervention specialist who may either attend your intervention, if you prefer, or simply help you develop your plan. Each intervention is unique just as each person is. You are likely to have questions that pertain specifically to your loved one’s circumstances. An interventionist can advise you about how to create a plan that’s poised for success. These professionals have been involved with numerous interventions; they can help you create a plan that’s tailored to your loved one’s situation.
Practice
Finally, rehearse your plan if possible. Be aware of who will lead the meeting. When you sit down to meet, it’s important that you have a very clear idea about what each of you will say so that you can make your intervention effective–and keep it on track.
How to Define Success
There are numerous possible outcomes for a mental health intervention. Every individual and mental health condition is unique and is influenced by a myriad of internal and external factors. This can make it challenging to recognize what a good outcome looks like.
Ideally, the individual will acknowledge that they have a mental illness and that receiving professional treatment will improve their condition and quality of life, and they’ll follow the treatment plan laid out for them. However, this isn’t the only “good” outcome. In some cases, a successful intervention may be one where the individual has an opportunity to talk openly about their mental illness and the participants can address stigmas surrounding mental health and treatment. While some people may only require one conversation before they seek treatment, for others, many conversations are needed.
Get Intervention Assistance with FHE Health
FHE Health specializes in mental health treatment.If you have any questions regarding the mental health intervention process or you’d like to speak about arranging a meeting and setting up a plan to help a loved one with mental illness, contact us today.






