This article has been reviewed for accuracy by our peer review team which includes clinicians and medical professionals. Learn more about our peer review process.
It’s not uncommon for people who have conditions like autism or ADHD to try to mask their diagnoses or even the way they normally behave or process information. In a world that seems to have clear definitions and rules for what “normal” means, there’s long been a stigma associated with many mental health conditions. However, the way many people approach some conditions that have historically been labeled impairment or disability is changing or, at least fueling conversations about how we should approach certain conditions. To that end, even the language we use can impact how we think about conditions like autism and how those who have these conditions may think about themselves.
New Vocabulary Terms to Describe Mental Health Differences
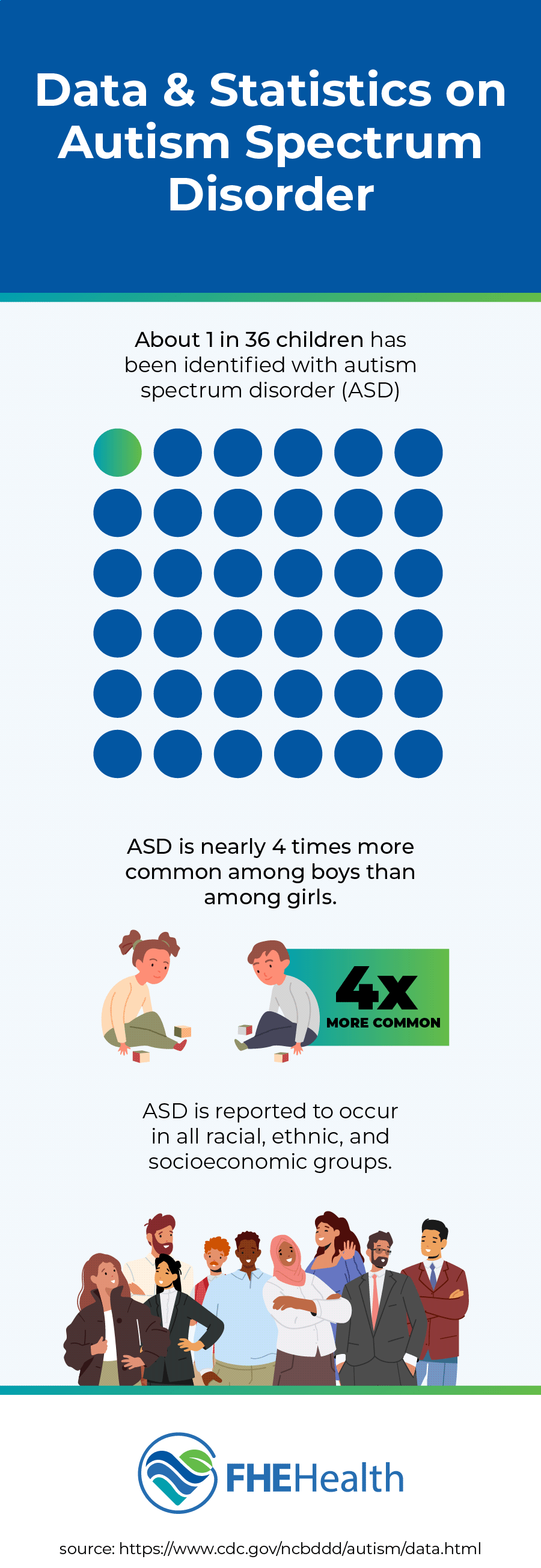
The medical community, as well as an increasing number of people in the public, are using new terms to describe people with mental health conditions such as autism and ADHD. Terms such as “neuroatypical,” “neurodivergent,” and “neurodiverse” highlight the fact that many humans have brains that are “wired” a bit differently from others. In fact, in the United States alone, 1 out of every 36 children was diagnosed with an autism spectrum disorder in 2020.
That statistic and the high prevalence of autism spectrum conditions imply that these conditions aren’t rare and occur with normal frequency, so much so that scientists have begun to regard them as normal brain variations. This has led the medical community to use terms like neurodivergent to highlight that brains with these conditions are different and not necessarily worse than those with neurotypical brains.
The common use of these new terms is spreading beyond the medical setting. Using neurodivergent to describe a person with ADHD, for example, has increased in many parts of the country, especially on social media. Why is the use of new terms to describe conditions that have historically had negative connotations more healthful? For one, these new terms help people recognize that they’re different but not less.
Second, negative labels can be a barrier to treatment. Fearing a negative diagnosis, many people don’t seek mental health treatment, even though it can improve their quality of life in many ways. In fact, there’s even been a push to change the name of conditions like schizophrenia to new terms that aren’t associated with stigma.
What Do These New Terms Mean?
Let’s explore what these new terms mean.
Neuroatypical
If a person without a mental health condition like autism is neurotypical, neuroatypical is the opposite. That is to say, a person with a neuroatypical brain has a brain structure that’s different from what the medical community views as normal or neurotypical.
Neurodivergent
Neurodivergent goes a step further. It, too, is often used to describe people with autism spectrum disorders, but it has a better connotation than neuroatypical. The true meaning of neurodivergent suggests brain divergency, not abnormalcy.
Neurodiverse
Neurodiverse is a term that began to be used during the 1990s and continues to be popular among medical practitioners and others. It, too, describes people with mental health conditions on the autism spectrum or ADHD. It highlights the idea that the human brain is quite diverse in its formation and function, particularly in regard to processing and behaviors associated with the conditions mentioned.
Neurological Variations
Neurological variations is an umbrella term used to describe the long list of conditions that might be considered neuroatypical. A sampling of the conditions on this list includes:
- Attention deficit hyperactivity disorder (ADHD)
- Autism
- Cerebral palsy (CP)
- Dyscalculia
- Dyslexia
- Obsessive-compulsive disorder (OCD)
- Tourette’s syndrome
Note that while many of these conditions are still labeled “disorders” or “syndromes” (for some of them, it’s right there in the name), the neurodiverse community has embraced the term “variations” to remove the stigma that’s long been attached to those who aren’t neurotypical.
Executive Function
Executive function refers to the various cognitive processes that govern goal-driven behaviors, such as reading, writing and carrying out activities of daily living. It includes working memory, planning, flexibility and emotional regulation. Neuroatypical conditions can impact executive function in different ways. For instance, people on the autism spectrum often experience social challenges, rigid thinking and sensory sensitivities. ADHD can cause difficulty with organization, focus and impulse control. Other executive functions commonly affected by neurodiversity include time management and adaptation to change.
Are Neurological Variations Disabilities?
Many neurological variations are still classified as disabilities, but a better way to think about them might be as different abilities. Although these variations can indeed affect executive function, they aren’t flaws or imperfections and can sometimes even enhance abilities. For instance, people with ADHD might struggle more than the average person to stay organized or focus on rote tasks, but they often can hyperfocus on areas of interest that others can’t. Autism might make it more difficult to thrive in certain social settings, but many people on the spectrum can approach difficult problems from unique perspectives and come up with innovative solutions.
What Is the Correct Language to Use?
Language is always changing and evolving, particularly in the way it’s used to describe various disabilities and the people who have them. When it comes to neurological conditions, the currently accepted terms are the ones described above: neurotypical, neuroatypical, neurodiverse and neurological variations. If you’re discussing a specific condition within the realm of neurodiversity, such as autism or ADHD, it’s acceptable to simply use the name of the condition.
Above all, keep in mind that it’s seldom necessary to label a person’s neurological characteristics. We’re all just human beings with a unique set of personality traits, strengths and weaknesses.
Changes to the Social Lexicon Can Be Positive
The use of these new terms can be positive. Language can affect the way we think about many different topics. Language can affect what we see. It can affect our opinions. We’re used to terms like “abnormal” having a negative connotation. On the other hand, a word like diverse has a positive connotation. Moreover, considering the prevalence of autism spectrum disorders, diversity is actually a more apt descriptor as these conditions occur with surprising normalcy.
Stigma and discrimination are not unknown to many who have been diagnosed with a mental health disorder. Consequently, it’s perfectly understandable why many people would want to avoid the use of labels that could be harmful to their well-being. Using these new, more positive terms is a helpful way to reduce the stigma associated with mental health disorders—and differences.
The Risk of Identifying with Overly Positive Terms
There is some risk with using overly positive terms to describe mental health spectrum conditions that we can’t overlook. Being neurodivergent should not imply that a person doesn’t require mental health treatment. The problem with using positive terms to describe mental health conditions comes with a risk that people may not recognize the necessity of seeking and continuing treatment to manage their condition–and management is often a necessity.
For instance, most of us have heard people refer to their brains as “wired differently” from the brains of others. They’re often talking about their quirks or individual habits as being neuroatypical or neurodiverse when, in actuality, they fall into the neurotypical spectrum of behaviors or processing.
If the use of positive terms prevents a person from seeking treatment for what they perceive to be as perfectly normal differences, that perspective could be damaging. People with autism spectrum disorders or ADHD typically require treatment to help them successfully manage and live with these conditions. Treatment can improve the way they function in the world and reduce their discomfort. That’s the goal of treatment, after all, to improve people’s quality of life.
Seek Help for Mental Health Today
While it’s ultimately a good thing to put a more positive spin on mental health disorders that have been associated with stigma, it’s also important to keep in mind that the use of new terms could “soften” the genuine need for treatment that these conditions require. Mental health terms are clinical in meaning for a reason; after all, they refer to medical conditions that generally require treatment. That said, with some conditions like autism spectrum disorder, these new terms can have a positive effect on people’s self-image and public awareness.
Regardless of perception and stigma, it’s important to seek treatment if you or a loved one needs it. Mental health issues can often be effectively treated with therapy, medication, and other treatments. If you or a loved one is experiencing any type of mental health problem, contact FHE Health to schedule an evaluation.