This article has been reviewed for accuracy by our peer review team which includes clinicians and medical professionals. Learn more about our peer review process.
It’s another busy morning for Dr. Nicholas Dogris, Ph.D., Director of Neurorehabilitation at FHE Health, on the day of our phone interview. Dr. Dogris directs the Neuro Rehab Services program at FHE Health, which is one of only a small number of providers in the nation to use neurostimulation and other cutting-edge brain technologies to address addiction and other mental health issues.
 On any given day, the specially trained team of neurotechnicians that Dr. Dogris oversees can be found administering different neurotherapy protocols, depending on the client’s symptoms, in one of FHE Health’s seven on-campus “neuro labs.” At times, the picture can look a bit like a scene from the sci-fit set of Stranger Things: With their head covered in electrodes, the client could just as well be entering a portal to another world; only in this case, they’re receiving a research-backed intervention proven to boost recovery outcomes and restore brain health. (Learn more about studies into the effectiveness of neuro rehab for symptoms of substance use and other mental health.)
On any given day, the specially trained team of neurotechnicians that Dr. Dogris oversees can be found administering different neurotherapy protocols, depending on the client’s symptoms, in one of FHE Health’s seven on-campus “neuro labs.” At times, the picture can look a bit like a scene from the sci-fit set of Stranger Things: With their head covered in electrodes, the client could just as well be entering a portal to another world; only in this case, they’re receiving a research-backed intervention proven to boost recovery outcomes and restore brain health. (Learn more about studies into the effectiveness of neuro rehab for symptoms of substance use and other mental health.)
Meanwhile, new innovations in the field of neurorehabilitation continue to expand the boundaries of what’s possible for brains in recovery. In addition to the services that FHE Health has been offering for a while now—EEG brain mapping, neurostimulation, neurofeedback—Dr. Dogris’ team has begun to use two more. What are they, and how do they work? Most importantly, what can they do for the person suffering from anxiety, depression, cravings, or other symptoms?
In the interview that follows, you’ll hear from Dr. Dogris in his own words about these two innovations in neuro care and discover why they offer good reasons to be optimistic about the future of behavioral healthcare….
Event-Related Potentials (ERPs)
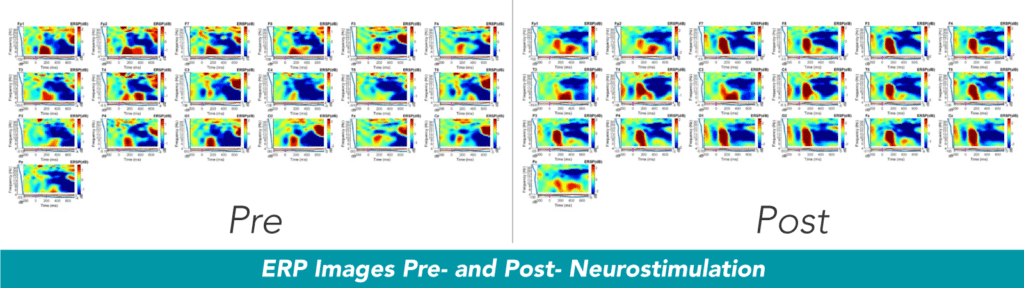
One groundbreaking advancement, event-related potentials, is “not treatment but a form of analysis … ERP’s have been around for a long time, but now new computational neuroscience analysis methods have brought them to the clinical EEG arena,” Dr. Dogris said. He explained that the standard neuro protocol has been to administer an electroencephalogram (EEG) that records brain activity. (In fact, there are two different kinds of this test: One is a 10-minute recording with eyes open, and the other is a 10-minute recording with eyes closed.)
These “standard measurements” in neuro care are “passive tests,” meaning they occur when the client is not doing anything apart from relaxing. Dr. Dogris drew a comparison to “listening to a car that’s idling, so when it’s idling right, it’s purring just the right way … if it’s going too fast or too slow, that alerts us to specific issues.”
In some cases, the client’s idling speed (or “peak alpha” in neuro terminology) is either too fast or too slow. This is when you’ll typically see symptoms, according to Dr. Dogris:
Anxiety, agitation, insomnia, anger, explosiveness—that’s when peak alpha is too fast. When it’s too slow, that can indicate a traumatic brain injury, blast injury, or emotional trauma.
Measuring How Fast the Brain Responds to Stimuli
“An ERP is an EEG,” Dr. Dogris said. “When we do the ERP, we’re recording the EEG.” The difference is that the ERP is looking at brain activity within a “go, no go” paradigm, where “you’re either hearing or seeing something.” For instance, “when you see two images on a screen, you click, and if you don’t see them, you don’t click … And in the ERP, we can label the electrical potential that’s positive or negative related to that specific event.”
We can also see how long it takes for a signal to move through the brain. For example, if it’s a visual signal, that visual signal “travels to your eyes and then the thalamus, which projects it out to your visual cortex and visual association areas—this is all simultaneous—also to your auditory cortex and motor cortex. (These regions all get that visual stimulus.)”
Why is being able to measure how fast a signal moves through the brain important? Here is how Dr. Dogris described it:
In neuroscience we have studied the “timing” of how long it takes for a stimulus to move from the eye to different parts of the brain. When the brain is damaged, it will automatically engage in neurogenesis, (a process by which dead cells are removed and new cells grow), and in this same process, the brain reroutes these signals and then the response to the stimuli takes longer.
Machine Learning for More Thorough Analysis
Another facet of ERPs that makes them groundbreaking: their use of a learning algorithm to analyze the data with much greater accuracy and specificity. (This form of factor analysis is called “AMICA,” and was developed by Jason Palmer at the Swartz Center for Computational Science at the University of California San Diego.) Dr. Dogris used the following metaphor to describe what this new AI-empowered, machine learning technology can do:
If we recorded 10 people talking at the same time, in the same room and fed this recording into AMICA, it would identify all 10 voices into independent components that allow us to examine each voice individually … Much like the voice, which has a spectral signature that’s unique, we can look at these specific signatures in the brain in 3-D. Once I know where a 3-D source is located, I can examine that source to determine if something is slowing down the processing of the brain. Once I know where it is and what it’s doing, then I focus on what we’ll do to stimulate the brain.
In these ways, the ERP is a “precise tool that allows us to look at brain issues and target where the issue is.” Dr. Dogris added that it is often useful in cases where an initial screening reveals significant brain injury, at which point one of the neuro team will recommend ERP testing.
Photo-biomodulation (PBM)
Among “the newest set of tools that we use,” according to Dr. Dogris, is a form of light therapy known as “photo-biomodulation” or PBM. It uses red and near-infrared light within the 650-1200 nanometer range to stimulate neurons. Light is energy, after all, Dr. Dogris explained, which “increases nitric oxide and reduces inflammation within the cellular structure. Also, ATP increases in the mitochrondia … That’s a big deal in helping the brain to heal itself.”
Existing literature suggests that photo-biomodulation has been effective for reducing cravings, inflammation, and symptoms of depression and anxiety. Meanwhile, Dr. Dogris and his team have been doing their own research into PBM’s effects while pairing it with cranial electrical stimulation and pulse electromagnetic field.
The Mental Health Benefits: What New Research Is Revealing
Thus far, their findings have been promising. After studying 4000 EEGs representing 1000 patients, Dr. Dogris found the following:
- Significant reductions in scores on the standardized anxiety measure GAD7 – Most clients begin treatment with a score of 15-20, and by Day 2 of receiving neurotherapy, their GAD scores were below 10.
- Significant reductions in scores on the standardized depression measure PHQ9 – By Day 3, clients’ scores had dropped and by Day 7, were below 5 points.
- A marked improvement in sleep – By Day 5, clients were sleeping through the night.
These outcomes, “as compared to controls who only received standard treatment,” were “significantly better.” In fact, clients who received PBS with neuro treatment experienced “double the treatment effect,” Dr. Dogris said.
Such results, however preliminary, offer new hope for quicker, more comprehensive relief of mental health symptoms like anxiety, depression, and insomnia. The full extent of the mental health benefits of photo-biomodulation remain to be seen. For now, though, it takes its place next to event-related potentials as yet another encouraging breakthrough in neuro care.