
People with mental health disorders and their loved ones sometimes wonder whether therapy will really help— maybe especially within the more intensive counseling context of an inpatient mental health program. Many of these same families face the added challenge of evaluating mental health programs for their quality and effectiveness, and it’s not always clear what mental health services to look for when vetting a prospective behavioral health program.
Few people are as qualified to address these common concerns as Dr. Michael Jochananov (affectionately called “Dr. J”). In this second installment of a far-reaching interview—catch the first segment here—he responded to these and other concerns with some helpful, applicable insights for anyone who may be wondering whether they could benefit from counseling/therapy/mental health treatment.
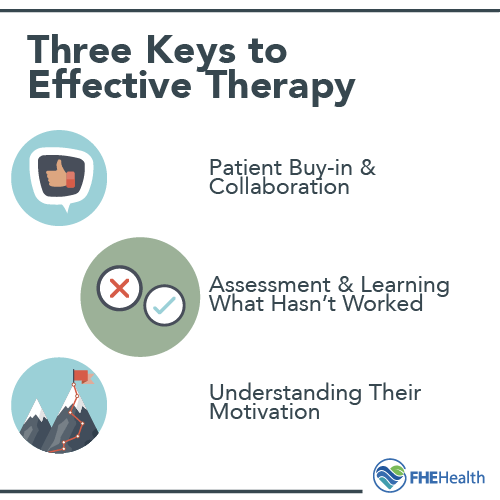
Three Keys to Effective Therapy
In Part 1 of the interview, Dr. J. talked about what defines quality treatment— a hallmark feature being evidence-based therapies that work.
Patient Buy-In and Collaboration
 On this note, Dr. J. said that “having patients’ buy-in is critical” to the success of inpatient therapy and is, therefore, a point of emphasis in his oversight of the development and management of patient treatment plans. The patient-centered approach is along the lines of “we understand that you [the patient] are the expert on yourself, and we [the staff] are the experts on the emotional and behavioral issues, so we need to work collaboratively.”
On this note, Dr. J. said that “having patients’ buy-in is critical” to the success of inpatient therapy and is, therefore, a point of emphasis in his oversight of the development and management of patient treatment plans. The patient-centered approach is along the lines of “we understand that you [the patient] are the expert on yourself, and we [the staff] are the experts on the emotional and behavioral issues, so we need to work collaboratively.”
Dr. J. said he encourages the clinicians whom he supervises “to help patients become an active part of their treatment” and “to challenge patients in measurable ways.” A case in point: “Focus on treating symptoms rather than diagnosis.” Dr. J. explained how:
Patients come in and say “I am bipolar,” and I encourage them to think beyond the labels … We want to know what their specific symptoms are. Maybe their symptoms are irritability, an inability to sleep and bad choices. Then we can focus on those symptoms and get them to buy-in.
In other words, an effective therapy will solicit a patient’s buy-in and motivation to recover. It will also do the work of exploring beneath the label of a diagnosis to address the individualized symptoms at play.
A Detailed Assessment and Identifying a Person’s Motivation for Recovery
Here are two more keys to effective therapy, compliments of Dr. J.:
- “Digging into what has helped and what hasn’t helped [a patient’s symptoms]” – Conducting an in-depth assessment of the patient and really learning what hasn’t worked for them in the past can be a big leg-up in meeting their treatment needs.
- “Knowing what [the patient’s] motivation is and whether they’re here because they want to be”- Gauging a patient’s level of motivation at the outset can provide another entry point to understanding how best to help them.
What’s the Utility of Therapy?
For patients and families asking this question, Dr. J. encouraged a quick inventory of what, if any, therapies they may have already tried. (After all, there are many types of therapy, so if one hasn’t worked, another may.)
Realistic expectations are also important. Anyone who is uncertain about whether therapy is for them needs to know that “therapy is hard work and there is no magic pill,” Dr. J said.
Therapy also takes some degree of faith and courage. Dr. J. used a metaphor from a quote he once heard and paraphrased. “In order to reach new lands, you have to be willing to lose sight of the shore for a time,” the quote went.
Why Is Mental Health Treatment Important for Addiction?
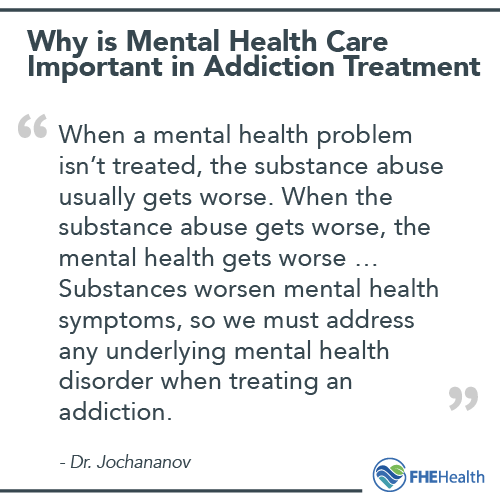 “It is important because both of these issues are co-occurring,” Dr. J. explained, adding:
“It is important because both of these issues are co-occurring,” Dr. J. explained, adding:
Both the mental health and addiction have their unique systems that get in the way of functioning on a daily basis; and, making the situation more complicated, is when they’re co-occurring. When a mental health problem isn’t treated, the substance abuse usually gets worse. When the substance abuse gets worse, the mental health gets worse … Substances worsen mental health symptoms, so we must address any underlying mental health disorder when treating an addiction.
A trusted behavioral health provider will “differentially diagnose” the conditions at play and “address which is in the forefront and treat accordingly.”
How to Find Quality Mental Health Treatment
 Dr. J. had these quick pointers to offer individuals and families affected by a mental health disorder:
Dr. J. had these quick pointers to offer individuals and families affected by a mental health disorder:
- “Do your research and see what’s out there … everything that glitters is not gold so to speak.
- Ask friends, people you know, etc., for input about where they went to treatment.
- Check Yelp and other reviews. See what others’ experiences have been and what they found helpful.
- Only pursue treatment that has stood the test of time and is research-based, such as CBT, Neurotherapy, and medication management, among others.
- Accreditation and certification of a prospective treatment program are extremely important as well.”
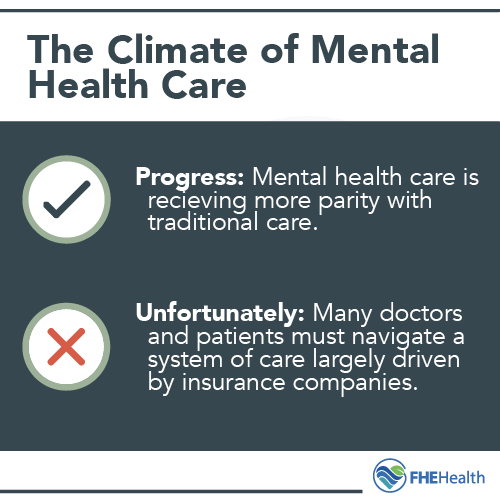
Important Trends in the Mental Health Industry
Current trends in the mental health industry seem to be a mixed bag of sorts for patients and families. On the more positive side, Dr. J. cited “greater parity with physical conditions, greater acceptance of mental health needs and less stigma, and new treatments.” He also lauded expanded mental health insurance coverage as another step forward.
On the flip side, Dr. J. lamented the fact that he and other behavioral health professionals must navigate a system of care largely driven by insurance companies. Here he used the example of long-acting, anti-psychotic injections such as Abilify and Risperdal. Like other treatments that are better both for the patient and the prescribing psychiatrist, these injections are not covered by insurance. Consequently, patients must choose between the treatment option that is better for them and the one that is covered by their health insurance plan.
Larger industry trends aside, Dr. J. is clear about what constitutes success for patients in FHE’s Mental Health Program. At the end of the day, “We know we’ve done a good job when they don’t need us,” he said.
Speaking of the same metric of success as it applies to staff, he said, “We’re successful when we’re not needed anymore and when we teach these patients to be their own therapists in their life … We want them to be self-sufficient.”






