
Who Is at Risk for Mental Illness?
Mental illness is a biopsychosocial disease with a strong genetic component. If a parent, sibling or grandparent is diagnosed with a mental illness, the likelihood of developing the same or similar kind of mental illness does increase. Although the exact etiology of mental illness has not been established, it is generally accepted among mental health professionals that specific factors impacting a person’s childhood strongly correlate with development of a mental disorder. These factors include but are not limited to:
- Having family members with mental illnesses or personality disorders
- Being verbally, sexually and/or physical abused
- Failing to graduate high school
- Having lower economic/social status
- Living in an unstable, dysfunctional and/or authoritarian family environment
- Being neglected, bullied or subjected to trauma
Some studies involving mental illness and identical twins indicate that environment may play a significant role in the development of mental illness. Longitudinal research following identical twins throughout their lives concluded that if both twins carry genes for schizophrenia but only one twin becomes schizophrenic, something in the schizophrenic twin’s environment may have “triggered” the gene. Similar results have also been observed in people with depression, anxiety and other mental illnesses.
What Is a Genetic Mental Disorder?
 Genetic disorders occur when abnormalities emerge in the unique genome of an individual. Genetic disorders are inherited when defective genes from one or both parents are passed to offspring. In some cases, a genetic disorder is simply a novel change (mutation) affecting a person’s DNA.
Genetic disorders occur when abnormalities emerge in the unique genome of an individual. Genetic disorders are inherited when defective genes from one or both parents are passed to offspring. In some cases, a genetic disorder is simply a novel change (mutation) affecting a person’s DNA.
Single gene disorders resulting from one mutated gene constitute nearly 4,000 diseases currently known to exist. Capable of being passed down through many generations, single-gene disorders involve dominant and recessive gene types, with genetic disorders depending on “recessive” genes lying dormant for three or four generations before they inexplicably emerge again.
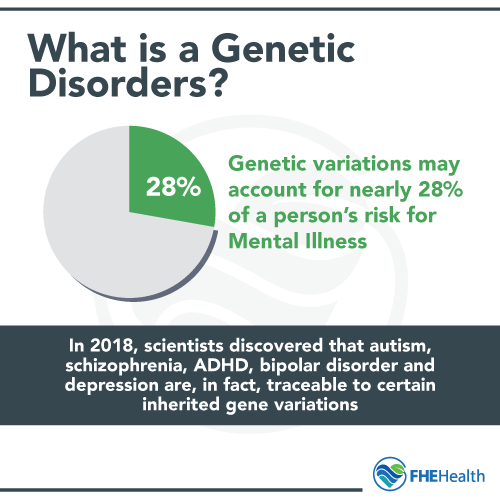
In 2018, scientists discovered that autism, schizophrenia, ADHD, bipolar disorder and depression are, in fact, traceable to certain inherited gene variations. Results of a large genome-wide study found that these genetic variations may account for nearly 28 percent of a person’s risk for mental illness.
Scientists also learned that shared variants such as mutations, deletions, duplications and gene-environment correlations further contributed to the emergence of mental disorders. In addition, studies suggest there may be an overlap among these five mental disorders, meaning some genes may carry markers for multiple mental illnesses.
What Triggers Genes for Mental Illness?
Why do some people with a genetic predisposition for mental illness eventually suffer from schizophrenia or bipolar disorder while others do not? An article published in the July 2003 Science described study results showing adolescents and young adults who experience stressful situations (relationship breakups, losing jobs, death of a parent or sibling) are prone to suffering major depression, especially if they inherited a specific type of serotonin transporter gene involved in brain cell signaling and communication. In addition, functional magnetic resonance imaging scans revealed that people with this gene variant demonstrated hyperactivity in a brain area (amygdala) that processes anxiety and fear.
Scientists hypothesize that young adults with variations in the serotonin transporter gene may see the world as a scarier, more menacing place than those without the gene variant. Therefore, stressful events that most people cope with productively are heightened to the point of causing major depression.
Genetics and Depression
 People who suffer from chronic depression rather than temporary, stress-induced depression almost always have a family history of depression. Family members of chronically depressed individuals are often found to have been diagnosed with some form of depression or other mental illness, such as bipolar or a schizotypal disorder.
People who suffer from chronic depression rather than temporary, stress-induced depression almost always have a family history of depression. Family members of chronically depressed individuals are often found to have been diagnosed with some form of depression or other mental illness, such as bipolar or a schizotypal disorder.
However, this association remains unclear. Scientists still do not know whether a single depression gene exists or if depression is the result of dysfunctional interactions between family members. Determining genetic risk factors for the different types of depression is challenging and perplexing. For example, depression could actually be a constellation of multiple disorders presenting different but strikingly similar symptoms. This means each type of depression could have diverse, multilayered genetic risk factors.
Genes thought to correlate with depression perform different functions in the brain. Some “depression” genes control the synthesis, activity and transport of neurotransmitters, while other genes regulate maintenance and growth of neurons. Depression genes may be triggered by drug addiction, alcoholism, physical/emotional abuse, disturbing life events such as divorce, deaths or long-term unemployment) and even the stress of dealing with a severe chronic disease. Currently, ongoing research supports the theory that the interplay between genetic and environmental factors is the primary factor increasing a person’s risk for developing major depression.
Is Bipolar Disorder Genetic?
 Scientists began suspecting mental illnesses may be genetic over 30 years ago after conducting the first twin studies involving schizophrenia. Bipolar disorder also appears to have a genetic component involving gene variations responsible for coding cellular operations that regulate calcium flow to brain cells.
Scientists began suspecting mental illnesses may be genetic over 30 years ago after conducting the first twin studies involving schizophrenia. Bipolar disorder also appears to have a genetic component involving gene variations responsible for coding cellular operations that regulate calcium flow to brain cells.
The CACNA1C gene variation found to play a key role in the development of bipolar disorder is also associated with depression and schizophrenia. It further regulates brain activity involved in cognition, emotion, memory and attention — all functions impacted by mental illness.
Researchers have also discovered variations in specific areas of chromosome 3 and chromosome 10 in people with bipolar disorder, schizophrenia and depression. However, it is the variated region in chromosome 3 that presents the strongest correlation to bipolar disorder in genetic studies.
Children and teenagers at risk for bipolar disorder because they carry certain genes may also be more sensitive to stressors than children without the gene. In addition to life event stressors, other things that could trigger bipolar genes in children under 18 years old could involve diet, abnormal sleep/wake cycles and serious viral illnesses.
The Bottom Line: Is Mental Health Hereditary?
The answer to that question is a confusing yes and no. Just because you inherit genes for a mental illness doesn’t mean you will eventually be diagnosed with that illness. Although genetic testing cannot give you an accurate prediction regarding your risk for suffering a mental illness, you may be able to take preventative actions if there is a history of mental illness in your family. Counseling and psychoeducation can be immensely helpful to those at risk for mental illness. Seeing a therapist when you are under extreme stress is also an excellent way to help you cope with unpleasant events complicating your life.
Call us today if you would like to learn more about the heritability of mental health conditions. We have understanding, experienced counselors who will discuss your concerns and help you make decisions beneficial to your psychological well-being.






