Humans are capable of feeling and expressing a wide range of emotions, from joy at a wedding to grief when a loved one passes away. If you suffer from emotional blunting and apathy, though, it may seem like you’re unable to feel anything at all. In this guide, learn the causes and effects of emotional blunting and the available treatment methods so you can feel like yourself again.
What Is Emotional Blunting?
 Emotional blunting, also called reduced affect display, is a condition that makes it difficult for sufferers to feel positive or negative emotions. People with this condition may feel apathetic, as though their life is dull, flat and meaningless, which can be very distressing. They might be unable to enjoy hobbies they once loved, laugh at jokes or cry when something sad happens. If asked to describe how emotional blunting feels, sufferers might say they are “empty” or “numb.”
Emotional blunting, also called reduced affect display, is a condition that makes it difficult for sufferers to feel positive or negative emotions. People with this condition may feel apathetic, as though their life is dull, flat and meaningless, which can be very distressing. They might be unable to enjoy hobbies they once loved, laugh at jokes or cry when something sad happens. If asked to describe how emotional blunting feels, sufferers might say they are “empty” or “numb.”
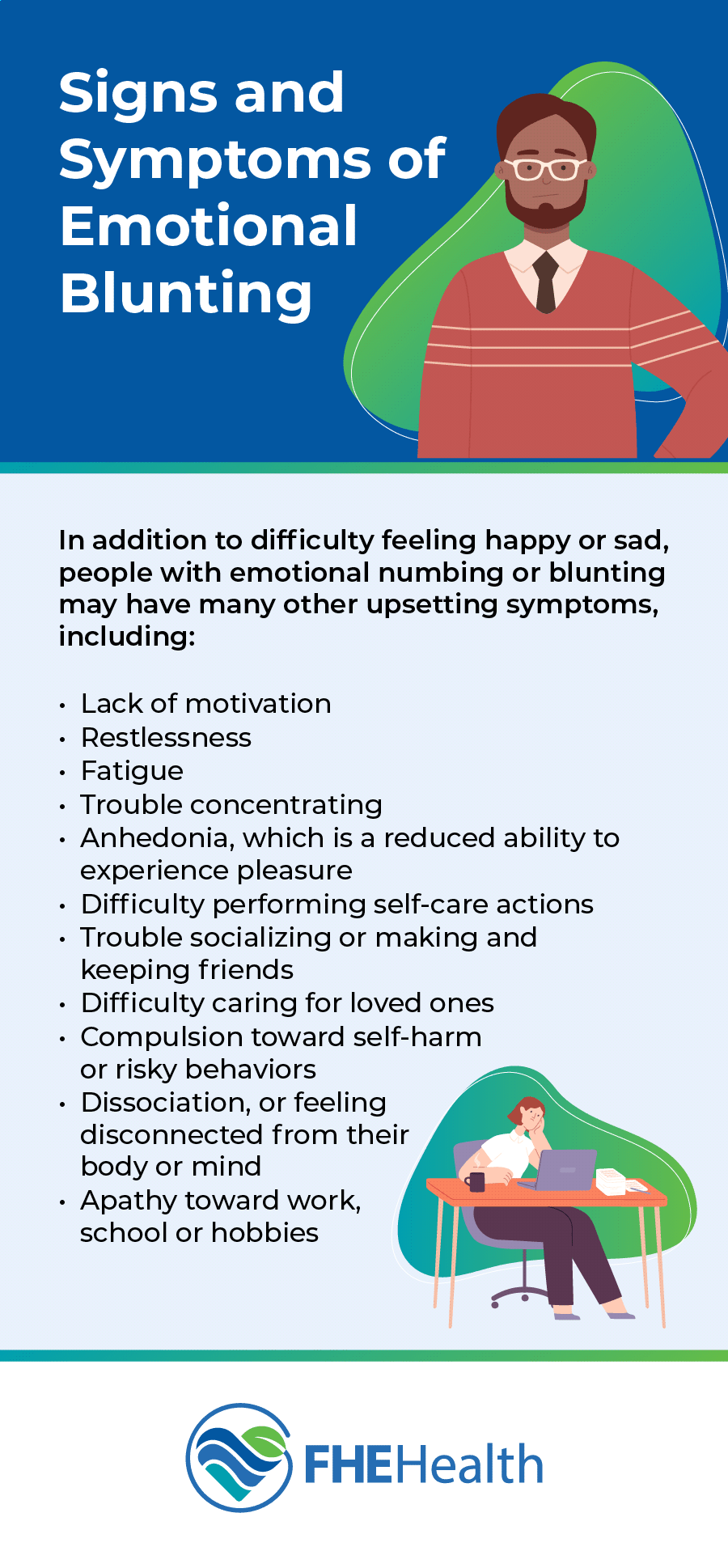
Signs and Symptoms of Emotional Blunting
In addition to difficulty feeling happy or sad, people with emotional numbing or blunting may have many other upsetting symptoms, including:
- Lack of motivation
- Restlessness
- Fatigue
- Trouble concentrating
- Anhedonia, which is a reduced ability to experience pleasure
- Difficulty performing self-care actions, such as showering and eating healthy meals
- Trouble socializing or making and keeping friends
- Difficulty caring for loved ones
- Compulsion toward self-harm or risky behaviors in an attempt to feel something, even if it’s negative
- Dissociation, or feeling disconnected from their body or mind
- Apathy toward work, school or hobbies
Causes of Emotional Blunting
 Emotional blunting can have many causes, one of the most common being depression. People who are depressed don’t always feel sad — rather, many sufferers become apathetic and find it difficult to care about anything in their lives. This effect is especially pronounced in people who take antidepressant medications, such as selective serotonin reuptake inhibitors (SSRIs), which are used to boost serotonin levels in the brain. One study found that up to 60% of people taking these medications experienced blunting as an antidepressant side effect.
Emotional blunting can have many causes, one of the most common being depression. People who are depressed don’t always feel sad — rather, many sufferers become apathetic and find it difficult to care about anything in their lives. This effect is especially pronounced in people who take antidepressant medications, such as selective serotonin reuptake inhibitors (SSRIs), which are used to boost serotonin levels in the brain. One study found that up to 60% of people taking these medications experienced blunting as an antidepressant side effect.
Dissociative Disorders and Emotional Blunting
Emotional blunting is also seen in dissociative disorders, such as derealization and depersonalization. People with derealization feel detached from their surroundings, while those with depersonalization feel they’re observing their life from an outside perspective. Dissociative disorders are uncommon, but for sufferers, symptoms can be severe enough to prevent them from living a normal life.
Dissociation usually develops as a self-defense mechanism against extreme stress. Causes include:
- Witnessing or being a victim of domestic abuse
- Childhood neglect
- Having a mentally ill or severely disabled parent
- Unexpected death of a loved one
- Severe stress caused by problems at work, relationship conflicts or financial trouble
- Use of hallucinogens, ketamine, marijuana and other illicit drugs
PTSD and Emotional Blunting
Another potential cause of emotional blunting is post-traumatic stress disorder (PTSD), which affects approximately 3.5% of U.S. adults each year. Many people associate PTSD with combat veterans, but this disorder can affect anyone who’s experienced a highly upsetting event. PTSD triggers can include domestic abuse, bullying, natural disasters, serious accidents and being a victim of a crime.
People with PTSD may develop emotional blunting as a way to protect their minds from the difficult things they’ve witnessed. Sufferers can feel detached from others, have negative reactions to loud noises and experience flashbacks or nightmares of distressing events.
Substance Use and Emotional Blunting
People who overuse alcohol can have difficulty feeling emotions, too. Alcohol blunts emotions by depressing the central nervous system. Drinkers may find this comforting at first but can quickly develop a dependence on alcohol as a way to avoid negative feelings and thoughts.
Neurological and Psychological Disorders
Certain neurological disorders, such as Alzheimer’s and related forms of dementia, can also have an effect on a person’s ability to feel emotion. A 2010 study found that elderly people with Alzheimer’s experience more emotional blunting compared to healthy individuals of the same age.
Other causes of emotional blunting can include schizophrenia, borderline personality disorder (BPD), schizoid personality disorder and alexithymia, a mental health condition that makes it difficult to express and understand emotions.
Treatment Options for Emotional Blunting
To treat emotional blunting, your doctor will first want to determine what’s causing your apathy and lack of feelings. This will help them choose a treatment plan that works for their unique needs. The diagnosis may include:
- Physical exam and blood work
- Review of your medical history
- Review of medications you’re taking
- Questions about drug and alcohol use
- Screening for depression and other mental health conditions
If you’re taking an SSRI, your doctor may suggest lowering the dosage or trying a different medication to help combat emotional blunting. Many people who stop taking antidepressants find they can feel emotions again once the drugs are gone from their system. However, it’s important to talk to your doctor before quitting any medication. Abruptly stopping antidepressants can cause unpleasant withdrawal effects, such as nausea, insomnia, sensory disturbances and flu-like symptoms.
If no physical cause for emotional blunting can be found, your doctor may refer you to a mental health professional, such as a psychologist or psychiatrist. If your apathy is caused by a psychological condition, a mental health professional may recommend therapy, medication or both.
Coping Strategies for Emotional Blunting
Talk therapy is an excellent coping strategy to help you deal with the effects of emotional blunting. A talk therapist can help you understand why you might be feeling numb and give you tools to overcome apathy. A talk therapy session may include:
- Discussing past and current events that are troubling you
- Finding healthy ways to cope with stress and solve problems
- Using cognitive behavioral therapy (CBT) to change negative thought patterns into positive ones
- Identifying a support network of trusted people you can turn to for help
- Guidance for people who self-harm or are having thoughts of suicide
If your emotional blunting is caused by certain triggers or events, a therapist may try exposure therapy to lessen the impact these situations have on you. Exposure therapy can be especially helpful for people with PTSD and anxiety.
Get Support and Treatment at FHE Health
When you’re ready to take the next step in treating your emotional blunting, contact us at FHE Health. Our counselors are standing by to guide your recovery and help you live the life you deserve.