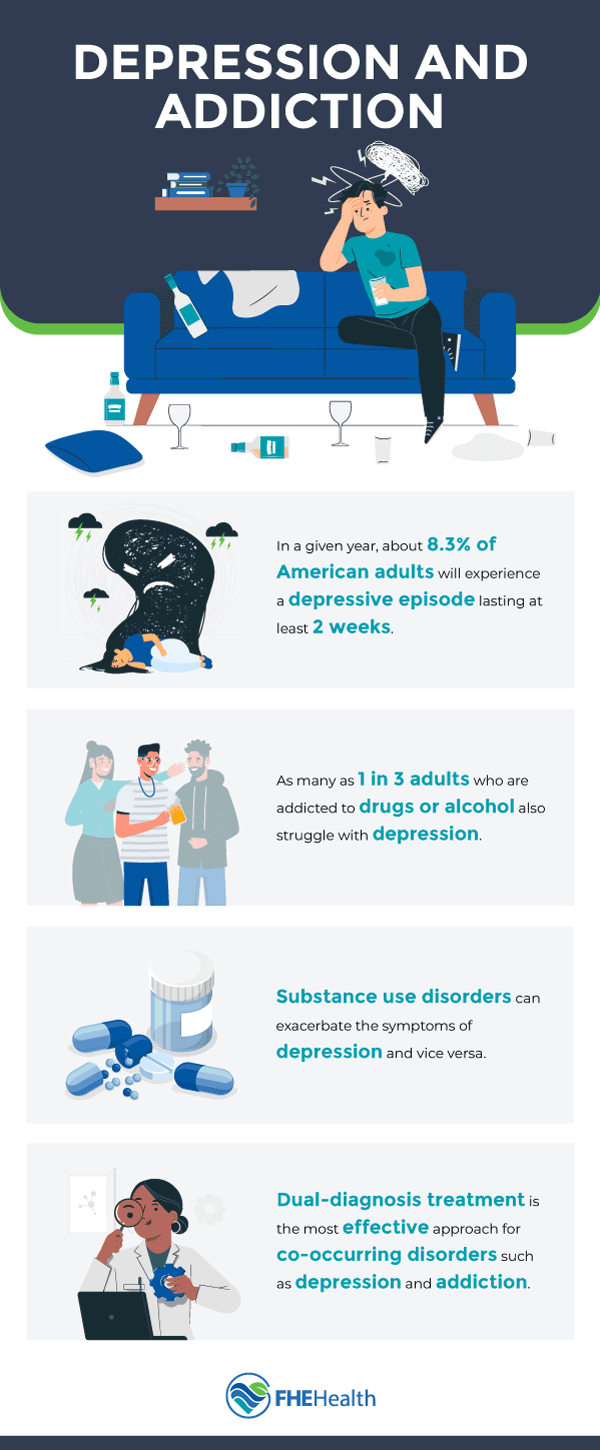
Depression and addiction often occur together, and people can be left wondering, does one cause the other? Which one happens first? The truth is, they’re closely related and it’s possible for substance abuse to exacerbate depression, while people with depression often turn to substances to self-medicate. It’s a complex situation that must be handled with care.
People with co-occurring depression and addiction often need to treat both conditions concurrently to manage either. If their substance abuse is motivated by underlying depression, treatment for just the substance abuse isn’t as effective. Likewise, if their depression is treated, they may still have to grapple with the substance use disorder afterward.
Understanding the Link Between Depression and Substance Abuse
 Depression is a common diagnosis for those who abuse substances. One study found that 23.4 percent of men and 48.5 percent of women dependent on alcohol are diagnosed with major depression at some point in their lives. However, clinical samples show an even higher rate of co-occurrence, somewhere between 50 and 70 percent.
Depression is a common diagnosis for those who abuse substances. One study found that 23.4 percent of men and 48.5 percent of women dependent on alcohol are diagnosed with major depression at some point in their lives. However, clinical samples show an even higher rate of co-occurrence, somewhere between 50 and 70 percent.
Further statistics show that half of people with substance use disorder also have some sort of co-occuring mental health condition. In the medical world, this is known as a “dual diagnosis.” Dual diagnoses can further complicate treatment for both the addiction and the underlying mental health condition, making it essential for medical professionals to have a full picture of a person’s mental health before ever engaging in rehabilitative treatments for addiction.
In part, this is because common risk factors exist for both substance abuse disorder and depression. These include trauma, stress and genetics. However, having a mental health disorder like depression also increases the risk of someone developing substance abuse disorder.
How Depression Fuels Addiction Cycles
Addiction can cause depression, or at least contribute to its development in people who are already predisposed to it. Addiction can also reveal underlying mental health conditions that were always somewhat present, but never manifested in a way that the symptoms affected day-to-day life.
Some people with depression use substances like alcohol or illicit drugs as a way to self-medicate their symptoms. Depression commonly presents with symptoms such as:
- Persistent sadness or feeling empty
- Losing interest in enjoyable activities
- Feeling hopeless
- Feeling irritable or frustrated
Many substances alleviate these symptoms short-term, using them for a reprieve from the discomfort. However, for people with depression, the rewarding effects, such as euphoria or relaxation, can also increase the likelihood of developing a substance use disorder. This creates a cycle in which the individual may consume more of the substances to cope with the increasing symptoms while also making their symptoms worse when not using.
For example, alcohol increases dopamine levels in the brain, which is why people who consume it feel good short-term. However, alcohol can cause depression by also disrupting serotonin levels in the brain.
Cannabis, commonly known as marijuana, is another substance regularly used by people with depression for self-medication. However, it can also increase the risk of developing depression for those with a predisposition to it.
The Challenges of Dual Diagnosis Treatment
Dual diagnosis treatment poses several challenges for those pursuing recovery, but they can be managed by a knowledgeable team in the right environment. Common challenges include:
- Undiagnosed symptoms: Substance use disorders and depression can have overlapping symptoms that may result in a treatment provider missing the depression diagnosis altogether. However, if the underlying mental health condition is a major contributor to an individual’s substance use in the first place, it will be difficult to fully and successfully treat the substance use disorder. For example, someone with undiagnosed depression may use alcohol or other substances to self-medicate, which can mask some of their underlying mental health symptoms. Because those symptoms go undetected, they don’t get treated.
- Insurance coverage: Mental health conditions aren’t as widely covered by insurance providers, which can pose a serious financial burden to someone seeking treatment. While substance use disorders are widely covered, the individual may be expected to pay entirely out of pocket for their mental health treatment, creating a difficult barrier to overcome.
- Disjointed treatment: In some cases, even when someone gets treatment for both their depression and their substance use disorder, a lack of coordination and integration between providers can make it difficult for either treatment to be as successful as possible.
- Lack of access to comprehensive resources: Some people may simply not have access to the resources necessary in their area to treat a dual diagnosis.
Effective Strategies for Recovery and Healing
Recovery and healing from addiction and depression often require a multi-faceted approach. This often includes:
Professional treatment: Professional treatment for depression and substance use disorder can occur concurrently. Many of the common methods used for either condition, including cognitive behavioral therapy (CBT) and dialectical behavioral therapy (DBT) can be tailored to address both issues, provided they’re both diagnosed accurately at the beginning. Professional therapy can help individuals learn to identify negative thought patterns and behaviors that exacerbate depression and substance abuse. In these treatment programs, individuals learn how to reframe their thinking and change their actions to support a healthier lifestyle.
In some cases, an individual might be best served by attending an inpatient rehab treatment program, where they have access to regular therapies and other treatments to support their recovery. This can be especially important for those struggling with addiction to substances that are dangerous to detoxify from, such as alcohol or opioids. In these supportive communities, patients have the medical supervision they need and can gain access to supportive medications that can alleviate some of the unpleasant symptoms of withdrawal.
Medication: Some people with depression require medication to manage their condition. Antidepressants can help restore a balance of the neurotransmitters that can contribute to depression. They commonly increase serotonin and noradrenaline, which can improve mood and alleviate symptoms. Not all people with depression require medication, but those who struggle to manage their symptoms with other methods often benefit from them.
Support systems: Even after initial detox and breaking the cycle of substance abuse, it’s essential to maintain progress and continually keep the addiction in check. Family members and friends can create an encouraging, supportive environment where this is possible. When struggling with a dual diagnosis, it’s essential to surround yourself with people supportive of your treatment and progress who can be your rock during hard times when relapse might be tempting.
Many people also find great success in maintaining their sobriety by attending support groups like Alcoholics Anonymous and Narcotics Anonymous. Other support groups for people struggling with depression can also be greatly beneficial.
You Don’t Have to Face Your Dual Diagnosis Alone
Having a dual diagnosis of depression and addiction can complicate your treatment plan, but don’t let it deter you from seeking help. With the right team, diligence and support, recovery is possible.
Better days await at the other end of your healing journey and our compassionate team is ready to guide the way. We know how important it is to have a treatment plan custom-tailored to your unique diagnoses and circumstances and we’re prepared to treat depression and substance abuse concurrently to help facilitate your recovery. Reach out today contact us online to get started with one of our many professionals well-versed in dual-diagnosis treatment.






