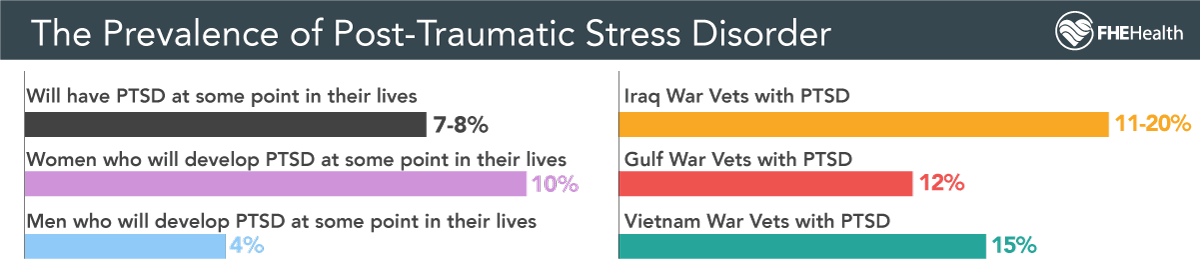
Post-traumatic stress disorder is a condition that stems from witnessing or being the victim of a violent event or other trauma. In the past, PTSD wasn’t widely understood, but today it’s recognized that as much as 6% of the population in the United States is suffering from the condition at any given time. PTSD from accidents might be one of the most common forms this takes, and the consequences can last a lifetime.
Because our understanding of PTSD is still developing, we’re still finding new common sources and triggers for the condition, including car accidents. Thousands of people have anxiety about driving (or even riding in) a motor vehicle because of a severe accident in their past that may have caused physical injuries. We’ll also discuss the other side of the event: emergency first responders who provide help at catastrophic car accidents and other fatal and life-threatening events.
Understanding the Ways PTSD Can Manifest
Post-traumatic stress disorder can develop after a person has been an up-close witness or a victim of a traumatic event. When someone is suddenly exposed to something jarring, the memories of the event can cause fear and anxiety about something similar happening. PTSD causes patients to exhibit irrational behavior in avoidance of these triggers and experience intrusive thoughts and dreams.
The Types of Violence That Causes PTSD
One of the most common situations that people associate with a high rate of PTSD is war, and for good reason. According to the VA, 15 percent of Vietnam veterans struggle with PTSD, and between 10 and 20 percent of veterans of the last few decades’ conflicts deal with the condition.
Here are examples of the violence and trauma that often results in the development of PTSD. It should be noted that after one of these events, PTSD isn’t guaranteed by any means, but it is extremely common.
- Rape and other sexual violence
- Up-close military violence
- Kidnapping and human trafficking
- Catastrophic accidents and natural disasters
- Terror and mass murder events
PTSD From Car Accidents
Post-traumatic stress disorder can develop after a person has been an up-close witness or a victim of a traumatic event. When someone is suddenly exposed to something jarring, the memories of the event can cause fear and anxiety about something similar happening. PTSD can cause people to exhibit irrational behavior in avoidance of these triggers and experience intrusive thoughts and dreams.
First responders are also at an increased risk for trauma-related illnesses simply because they frequently respond to traumatic events. A popular myth is that first responders are desensitized to violence, but studies find the opposite. For example, a systematic review of EMS mental health by the Agency for Healthcare Research and Quality, including a survey of more than 6,000 responders, documents widespread stress, compassion fatigue and burnout among first responders.
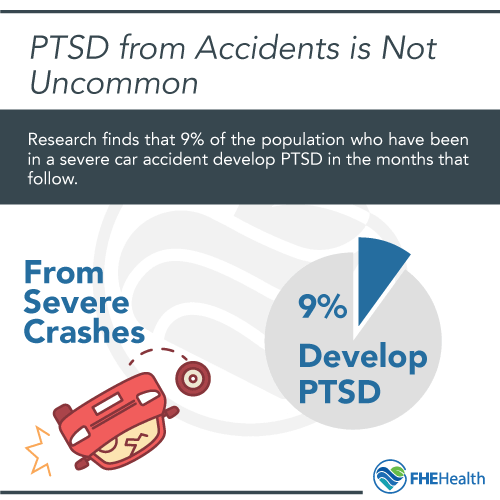
Update: recent research shows 39% of a study of Motor Vehicle Accident victims developed diagnosable PTSD.
Signs of PTSD After a Car Crash
PTSD from an accident can manifest in many ways, sometimes disrupting life long after injuries heal. Some survivors relive the accident through flashbacks, nightmares or intrusive thoughts that appear suddenly and feel vivid and real. Others avoid reminders of the crash, such as driving, certain intersections or even talking about what happened. Emotional symptoms may include:
- Anxiety
- Unexplained irritability
- Feelings of guilt
- A sense of detachment from others
Many people also experience physical reactions, such as a racing heartbeat, sweating or trembling when reminded of the event. Sleep problems, difficulty concentrating and sudden mood changes are also common. For some people who experienced a fatal accident, simply getting back into a vehicle or behind the wheel can cause extreme fear and anxiety. Other triggers can be more specific — something as common as another driver running a red light or the feeling of an abrupt stop can transport a person with PTSD back to their traumatic event.
PTSD can develop weeks or even months after car accident trauma occurs, which can make it hard to recognize what’s happening. The key sign is persistence. If distressing memories or emotional reactions don’t fade with time and continue to interfere with your daily routine, relationships or work, it’s worth reaching out to a mental health professional for evaluation and support.
First Responders to Car Accidents
 Not only do those involved in traffic accidents have a higher rate of PTSD, but so do the first responders who arrive on the scene to help. In general, first responders are at an increased risk for trauma-related illnesses simply because they frequently respond to traumatic events. A popular myth is that first responders are desensitized to violence, but studies find the opposite: 69 percent of EMS professionals reported that they didn’t have enough time to recover emotionally before having to respond to another grisly scene.
Not only do those involved in traffic accidents have a higher rate of PTSD, but so do the first responders who arrive on the scene to help. In general, first responders are at an increased risk for trauma-related illnesses simply because they frequently respond to traumatic events. A popular myth is that first responders are desensitized to violence, but studies find the opposite: 69 percent of EMS professionals reported that they didn’t have enough time to recover emotionally before having to respond to another grisly scene.
A notable example is the first responders to the wreckage in New York City immediately after the 9/11 terror attacks. There has been a public call for federal policymakers to approve an extension of a budget increase for these firemen, police officers and EMS, due to the long-term need to treat PTSD.
Triggers for Anxiety After an Accident
Depending on the circumstances of a car accident, triggers can vary greatly. For some who are involved in a fatal accident, simply getting back into the vehicle or behind the wheel can cause extreme fear and anxiety.
Other triggers can be more specific; something as common as another driver running a red light or the feeling of an abrupt stop can transport a person with PTSD right back into their traumatic event.
The Guilt and Shame Felt With PTSD
PTSD also commonly comes with feelings of guilt and shame, causing sufferers to dissociate, often resorting to drugs and alcohol to escape. Often, PTSD is internalized by the person suffering. They convince themselves that they were at fault for the initial trauma, even when there was no way to avoid it.
Some people feel PTSD caused by so-called lesser events, like a car accident, somehow makes them weaker. But PTSD isn’t something that can be controlled, and PTSD from a car accident is no less valid than PTSD from something “more serious,” like war atrocities.
The Consequences of Untreated PTSD
Left untreated, PTSD can be so severe that the person suffering from it becomes unable to accomplish daily activities and live a normal life. It’s one reason rates of homelessness are so much higher among veterans with PTSD than those without. Other consequences include:
- Mental illnesses like depression, anxiety and obsessive-compulsive disorder
- Addiction and substance use disorders
- Suicide
Treatment Options for PTSD From an Accident
There are several treatments people with PTSD from car accidents and other sources can undergo, with the aim of helping them become more comfortable with their triggers.
- Exposure therapy. A patient has controlled sessions where they’re gradually exposed to more and more of a specific stimulus.
- Counseling. A patient talks one-on-one with a counselor about their trauma.
- Support groups. People with PTSD get together to talk about their experiences and grow through a common recovery journey.
Considering inpatient treatment can be worthwhile in some cases. Learning more about what inpatient PTSD treatment is like can help.
Does It Vary From Other Treatments?
Exposure therapy has limited applications, but group meetings and one-on-one counseling for PTSD are similar to other mental health and addiction treatments. Each takes a different approach to helping patients learn about themselves and understand how they got to this point, with the goal of reducing anxiety about certain situations.
How Long Does PTSD Last After a Car Crash?
There’s no single timeline for recovery from PTSD after a car crash. Some people begin to feel better within a few months, especially with early intervention and a strong support network. Others experience post-accident anxiety and other symptoms that linger for years if left untreated. The duration often depends on factors like the severity of the crash, prior trauma, personal coping mechanisms and access to therapy or social support.
Evidence-based treatments such as cognitive behavioral therapy (CBT), exposure therapy and eye movement desensitization and reprocessing (EMDR) can significantly shorten recovery time by helping people process the trauma in a healthy way. Without treatment, symptoms may persist or even worsen, leading to chronic anxiety, depression or phobias about driving. Healing from PTSD is rarely linear — some days feel like progress, others like setbacks — but with the right care and patience, most people do recover.
FAQ
What’s the Most Severe Form of PTSD?
Complex PTSD (C-PTSD) is an especially severe type of PTSD. This form develops from chronic, repeated trauma and includes symptoms beyond typical PTSD, such as difficulty with emotional regulation and relationships.
How Can You Identify PTSD Triggers?
Everyone experiences PTSD from accidents differently, so there’s no one-size-fits-all list. It can help to keep a diary of your experiences and triggers to help you look for patterns in what triggers you.
Who’s Most Likely to Get PTSD?
Women are more likely than men to manifest the symptoms of PTSD. Research continues, however, and much has yet to be learned about how men process trauma differently from women.
Addressing PTSD at FHE Health
At FHE Health, we treat PTSD as well as a number of other mental health conditions. Our goal is to help you recover and be able to live a normal life. To learn more about your options, contact us today.






