
All military members play an integral role in maintaining the security of our country and the safety of its citizens at home and abroad, but when it comes to some of the most dangerous military operations, the special forces play a unique role. In the military, this is referred to as Special Operations Forces (SOF) and includes the following:
- Army Green Berets, Army Night Stalkers and Army Rangers
- Navy SEALs, Navy SEALs Missions and Navy SWCCs
- Marine MARSOC, Marine RECON and Marine RECON Missions
- Air Force Special Tactics
There are many myths about what SOF do and how they work, and much of this is because of how the media focuses on them in movies and TV shows. The media usually portrays SOF as going into a mission (that somehow only lasts a convenient 5 minutes or so) where everything is executed perfectly and the men and women involved become the heroes of the day.
The reality is that SOF missions start with a great deal of planning and strategy and can include days or weeks of waiting on the order to go in. This entire time, these teams are often in life-threatening situations, having to deal with enemy fire and the threat of landmines 24 hours a day. Rarely does real-life go off perfectly, and these soldiers may have to make split-second decisions in poor conditions and under extreme physical stress.
Many movies and TV shows also show soldiers getting out of the military only to return to a perfect civilian life without any transition issues. In reality, it’s very normal for veterans to need some time to adjust, just like with any major life change such as getting married or going away to college. The fact that the media doesn’t give accurate depictions of battlefield conditions, what it’s like to bet in the SOF or what a real transition back to a nonmilitary life means that soldiers and their friends and family may not be prepared for the realities of PTSD.
The Special Forces and PTSD
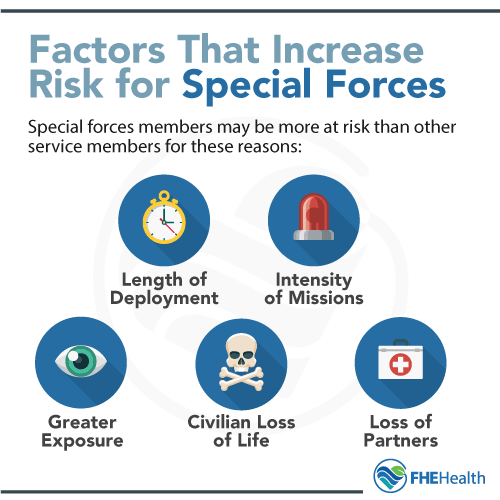 Special Operations Forces Members may be more at risk for PTSD than other service members. Some possible reasons for this include:
Special Operations Forces Members may be more at risk for PTSD than other service members. Some possible reasons for this include:
- The length of deployments
- The intensity of the missions
- The greater exposure to life and death situations
- Dealing with the deaths of civilians caught in the crossfire of missions
- Dealing with the deaths of fellow SOF members, whether in the field or to PTSD back home.
Things like directly facing a threat of death situation or witnessing another person go through traumatic events, such as a death or violent injury, dramatically increase the chances for PTSD. SOF are exposed to these things repeatedly, often over extended periods of time, which can take an incredible toll on their mental health.
Signs and Symptoms
While the signs and symptoms of PTSD can vary according to the individual and any strong change in personality should be considered a warning sign, here are some of the most common things to look out for:
- Experiencing flashbacks and nightmares
- Feeling numb or disconnected
- Avoiding people, places or events that may trigger unpleasant memories
- Difficulty focusing
- Difficulty sleeping
- Feelings of paranoia and hypervigilance
- Being easily angered or experiencing mood swings
- Inability to remember pieces or parts of certain events
It’s important to note that these symptoms are often delayed. Someone may return to civilian life (or just a deployment) and appear to be doing fine initially. It could take weeks, months or even years for PTSD to fully manifest.
Common Barriers to Seeking Help
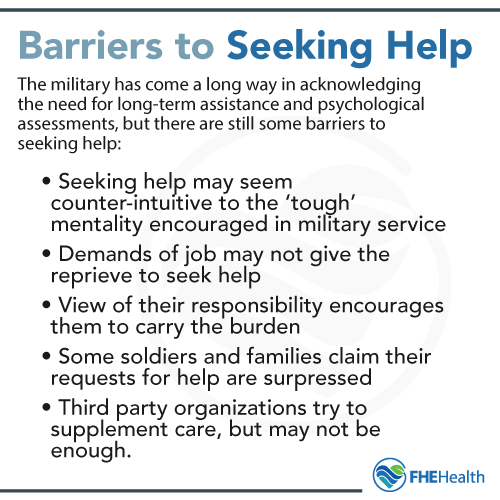 One of the biggest barriers to seeking help for PTSD is that military personnel are taught to be tough and to keep going no matter the conditions. While this serves them well in training and on the battlefield, it doesn’t always translate to long-term mental health.
One of the biggest barriers to seeking help for PTSD is that military personnel are taught to be tough and to keep going no matter the conditions. While this serves them well in training and on the battlefield, it doesn’t always translate to long-term mental health.
Active duty military and veterans may (incorrectly) feel like they are weak for experiencing the feelings and emotions they are and for not being able to just suck it up and move on. This, and the pressure to put on a good front and be tough can make it very difficult for them to admit the need and reach out for help. Some service members may also worry about their job security or losing their security clearance if they try to get help for PTSD symptoms.
The military itself also puts some barriers in place when it comes to seeking help for PTSD. Some soldiers and their families have come forward to tell their stories of being told to just deal with it or “keep it in the family” when they reached out to superiors for help. While there are programs like the Wounded Warrior Project and the Veteran Crisis Line, these resources aren’t always enough, especially if someone is hesitant to admit that there is a problem to begin with.
When US Special Forces PTSD Goes Untreated
Projects like Mission 22 have brought more awareness to the problem of suicide among service members and veterans, but it’s important to look at the numbers to understand what a serious issue this is. According to the U.S. Department of Veterans Affairs:
- Women veterans are 1.8 times more likely to commit suicide than nonmilitary females
- Male veterans are 1.4 times more likely to commit suicide than nonmilitary males
- Male veterans aged 18-34 have the highest suicide rate
- Male veterans 55 or older have the highest instances of suicide
- Almost 70% of veteran suicides are committed by firearm
Active duty military suicides were at record highs in 2018. Unfortunately, it’s a trend that doesn’t seem to be changing. While not all of these suicides may be PTSD related, many of them are, which is why it’s critical to seek help if you or someone you love is experiencing the effects of PTSD or is considering suicide.
At FHE Health, we understand that it can be hard to ask for help when you’re used to being the one who has to hold everything together, but being honest with yourself and your family and admitting that you can’t fix it alone is the first step. We have highly trained mental health professionals who can help you work through the traumas surrounding PTSD and learn coping skills to be able to go on to a better quality of life.






