“Integrated medical care” is a cutting-edge approach to behavioral healthcare. This collaborative care model for patient care employs an interdisciplinary team of medical and clinical health professionals who together treat the whole patient— not just the presenting mental health problem in isolation, but other medical issues as well, in order to achieve a better long-term recovery outcome for that patient.
Medically integrated treatment is not a common feature of the rehab landscape in America. Dr. Ahmed Howeedy, MD, MRO, the medical director at FHE Health, explained why in a recent interview. As Chief Medical Officer, he oversees the implementation of this approach to patient care across our various treatment programs at FHE Health. He, therefore, can speak with fluency about the integrated medical care model, and why it’s the most effective form of patient care for those with substance use disorders and other mental health conditions.
What’s So Cutting-Edge About Integrated Medical Care?
What, then, makes integrated medical care so “cutting-edge”? Here’s how Dr. Howeedy answered that question:
Historically, doctors are trained to identify a certain disease within a particular part of the body and target that specific process. Medical training developed that way regarding specific body systems and processes, and medical students learned that narrow targeted approach. Medical specialties developed within that framework as well, each working within their silo. While this method works for acute conditions, such as for bacterial pneumonia, it doesn’t work well for chronic conditions, which are not caused by one factor but rather many underlying factors involving many body systems. The truth of the matter is that each of those body systems do affect one another. Some pathology or imbalance in one does have a relationship with problems we see in other parts of the body. This is especially true for chronic conditions.
“Chronic conditions” include addiction, depression, bipolar disorder, post-traumatic stress disorder (PTSD), and other disorders that FHE Health treats. Their treatment—for most of history, even up until the present day—has been adversely impacted by what Dr. Howeedy calls a “divide between medicine and behavioral health,” such that “medical issues are often treated separately from behavioral health.”
“Historically, many places that have been adept at treating patients medically, but aren’t equipped to handle behavioral health issues, “Dr. Howeedy said. “Someone may go to the hospital with an acute medical issue and have it handled well, but [the same hospital] won’t do much for depression, insomnia, bipolar disorder, and vice versa: a person might go to a psychiatric facility and get good care for their psychiatric problem, but they won’t get good medical care for their diabetes.”
How Integrated Medical Care Improves Patient Treatment Outcomes
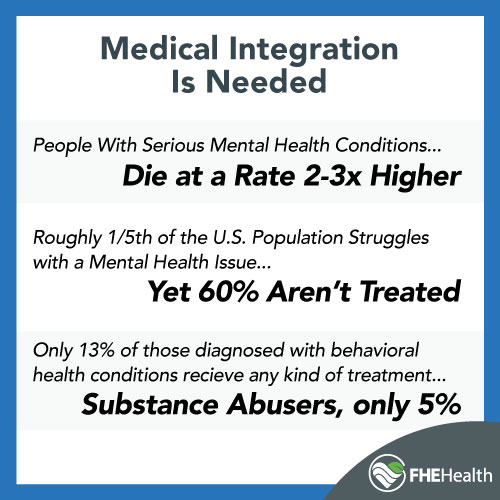
This prevailing divide between medicine and behavioral health has had “a lot of negative consequences” for patients, according to Dr. Howeedy. He noted, for example, research from the Kennedy Forum, which calls for more integration of the behavioral healthcare system with the medical system because of grim statistics like these:
- Patients with serious mental health conditions die at a rate that’s two to three times higher than that of the general population.
- Roughly one-fifth of the U.S. population struggles with a mental health issue, yet 60 percent of these Americans don’t get treatment.
- Only 13 percent of people diagnosed with a behavioral health condition receive minimally adequate treatment in a general medical setting; for substance abuse, that number drops to a dismal 5 percent.
Such statistics paint a depressing picture— but they aren’t inevitable. The same report makes the case that greater integration of the behavioral health system with the medical system would go along way to redressing these issues, by improving patient treatment outcomes.
Meanwhile FHE Health’s own research into recovery outcomes for addiction patients nationally has turned up similar findings: “Research was showing that to really improve patient outcomes, there has to be integrated care between medicine and behavioral health—the collaborative care model,” Dr. Howeedy said. Another takeaway: that “treatment centers can do better based on the high relapse and mortality rates for these addiction patients.”
Medically Integrated Treatment at FHE Health – How It Works and What to Expect
Medically integrated treatment at FHE Health is our effort to “do better” by every patient who comes through our doors. At FHE Health, patients have the reassurance that when they arrive at our facility, they will receive comprehensive medical treatment from a full team of doctors and nurses who will address all of their medical conditions, both the acute and the chronic. Why? Because “[patients’] medical conditions have a direct correlation with substance use disorders.”
In Dr. Howeedy’s words, “As we’re addressing [patients’] substance use disorder and mental health condition, we’re going to diagnose and treat their medical disorders.” This means “looking at undiagnosed medical conditions that might be contributing to their substance use disorder— and any medical conditions that have resulted from their substance abuse.”
As illustration, Dr. Howeedy gave the example of an 18-year-old heroin addict with Type 1 diabetes. (The condition, if left unmanaged, can cause glucose levels to skyrocket and trigger a coma— even death; it can also lead to chronic pain conditions like neuropathy that if left untreated can contribute to substance abuse.) Dr. Howeedy explained that if that heroin addict enters rehab and only receives care for his heroin addiction, he is not really any better off when he leaves rehab, in terms of his health and quality of life. Similarly, if only his diabetes gets treated, the physical and psychological causes of his heroin addiction will go unaddressed, almost guaranteeing that when he leaves treatment he will go straight back to using heroin.
As soon as they are admitted into one of our treatment programs, then, and up until their discharge, patients can expect to be followed by multiple specialists representing a spectrum of disciplines. Their care providers meet in daily interdisciplinary rounds to discuss patients’ treatment plans and how they are progressing. And, our medical providers share the same work space as our psychiatrists, which encourages close collaboration and integration of treatment plans.
Our Fully Equipped Medical Facility – and a Full Gamut of Medical Services
Another big advantage of integrated medical care for patients who come to FHE Health is that “our medical department can pretty much manage anything,” Dr. Howeedy said. “We can take patients whom most facilities are not equipped to take, as many patients have a difficult time finding a facility to treat their substance use or mental health conditions while at the same time being able to manage their diabetes, heart disease, COPD, chronic Pain issues, etc. We are able to provide our patients a full range of medical services whether it’s IV infusions, X-rays, EKGs, pulmonary function tests, hormone therapy, neuro-rehabilitative services, wound management, or minor surgical procedures. That’s a very unique thing in a treatment center.”
Because FHE Health is a fully equipped medical facility, we can offer a full gamut of medical services including the following:
- Round-the-clock medical care
- Medication management that ensures the correct medication(s), dosage(s), frequency of administration and duration of use
- Diagnostic testing, such as blood or serum analysis, EKGs, pulmonary function testing, X-ray and imaging, and minor surgical procedures
- IV vitamin infusions and IV hydration, which allow our medical team to address any nutritional deficiencies that may be affecting brain function and overall health
- Neuro rehabilitative services, such as brain scans that identify where there is neurological dysfunction and therapeutic brain stimulation that targets those regions
- Smoking cessation for patients who desire this— in the form of medications that can control cravings combined with therapy and counseling
- Weight management, through nutritional planning and fitness as well as yoga
- Massage therapy
- Acupuncture therapy
- Physical therapy
- Ketamine infusions for depression, obsessive-compulsive disorder, PTSD and even chronic pain syndromes
“Which of My Medical Conditions Gets Treated First?”
Because it is so common for patients with a drug or alcohol addiction or other mental health condition to have other underlying health issues, many patients want to know which of their conditions our medical team will treat first. Dr. Howeedy emphasized that while we will be looking at treating all of a person’s underlying conditions that may be contributing to their symptoms, we try to prioritize those conditions that are most acute that need to be stabilized, whether medically or psychiatrically:
Someone might have nutritional deficiencies and congestive heart failure, in which case while we would work to treat and stabilize their congestive heart failure, we would also be correcting their nutritional imbalances and working with a nutritionist to develop a personalized plan for them over the next few weeks— since both of these conditions can directly impact a person’s mental health and substance use. Heart conditions can affect the blood flow to the brain, and nutritional deficiencies can affect the function and neurotransmitters of the brain; so treating these conditions is essential in addressing their behavioral health conditions.
How Medically Integrated Treatment Has Helped Our Patients
Examples abound of how medically integrated treatment has helped patients with addiction and other mental health conditions. Dr. Howeedy recalled one example of a man who entered treatment: “he was hyperactive, couldn’t focus or concentrate, was skinny, losing weight and not eating, and had multiple nutritional deficiencies— and, because he wasn’t eating, he was dealing with a slew of medical conditions (skin issues, joint conditions, etc.).” Meanwhile, this man had been taking meth and opiates … But were the drugs really the reason for this man’s ailments?
Here is how Dr. Howeedy answered that question:
We found that the man had severe hyperthyroidism, and was producing so much thyroid hormone that his metabolism was on overdrive, which was why he couldn’t concentrate. People thought his problems were because of drug use, but the reality is he had a serious medical issue that could’ve killed him. Once our medical team was able to diagnose his thyroid problem, help him manage that imbalance, and attend to affected body systems (cardiac, liver, renal, GI, etc.), the patient began to gain weight and his symptoms began to improve … he found he did not need to rely on drugs to manage his symptoms, and he was also able to then learn healthy new coping behaviors [in place of the drug abuse].
The main conclusion that Dr. Howeedy draws from this example and many others is this:
At the end of the day, a person’s medical conditions will have a direct correlation with how their brain functions … The brain doesn’t float in its own little box. It’s sitting in a body with hormones, chemicals, nutrients, and toxins. All those things are affecting brain function, and if a person’s overall physiology is not maintained, that’s going to affect the brain, its neurochemicals, functions, neurocircuitry, and how the patient makes decisions in their life. The physiology of the body does have a direct correlation with the brain. The integrative care model recognizes this direct correlation.
For patients considering where to go for rehab, then, medically integrated treatment should be a decisive factor in the selection process.






