
Treating substance addiction with hallucinogens is a hot topic within the evolving field of addiction treatment modalities. Many people believe that using ibogaine treatment, ketamine or psilocybin can help people struggling with PTSD, depression or addiction.
Hallucinogens are drugs that cause audio, visual, tactile or olfactory hallucinations by disrupting neurotransmitter systems within the spinal cord and brain. Neurotransmitters that regulate sensory perception and mood include dopamine, serotonin, acetylcholine and norepinephrine.
Unlike heroin, cocaine or methamphetamine, hallucinogens don’t target the reward centers or opioid receptors in the brain. Instead, they stimulate chemicals and brain areas primarily involved in how we perceive things. This is why they’re not considered as addictive physically or psychologically as heroin, meth, cocaine, alcohol and opioid pain pills.
The Psychiatric Use of Hallucinogenics for Treating Drug and Alcohol Addiction
Advances in neuroscience and associated imaging technology allow researchers to study detailed data regarding the efficacy of hallucinogens for treating substance addiction. In particular, MRI and PET scans have made it easier to examine sites of action in the brain while someone is high on a hallucinogen.
Interest in the effects of psychedelics (now referred to as “club drugs”) as a way of treating mental illness isn’t new. However, the last few years have seen a resurgence in the research into and use of psychedelics as medicine. While there are still some unregulated drugs, others, including MDMA (Ecstasy) and psilocybin (mushrooms), are now used in the United States with permission from the Food and Drug Administration.
Although some hallucinogens have been shown to have beneficial effects on addicts with histories of chronic substance abuse, all club drugs are known to significantly alter brain chemistry, disrupt signaling between brain cells and possibly increase the risk of worsening depression, anxiety or severe mental illnesses such as schizophrenia.
Researchers still don’t fully understand exactly how LSD, Ecstasy and other psychedelic drugs impact brain functioning in the long term. While using hallucinogenics may relieve some addiction or withdrawal symptoms, there’s still the potential that the use or misuse of these drugs could do lasting damage to the brain. However, hallucinogenic substances do often encourage self-reflection, and many people credit them with bringing about a spiritual awakening, which can be helpful in the recovery process.
Some drugs that are used, in both regulated and unregulated environments, include:
Ecstasy (Methylenedioxymethamphetamine or MDMA)
Ecstasy is an amphetamine-based drug that substantially increases serotonin, norepinephrine and dopamine levels in the brain. A rapid, steep rise in these particular neurotransmitters makes people taking Ecstasy experience intense hallucinations involving all five senses. Euphoria and a feeling of oneness with others make MDMA a favorite of party-goers known as “ravers.”
While addicts may feel less depressed or discouraged when using Ecstasy to defeat their addiction, this club drug can cause serious psychological side effects due to serotonin neurotoxicity. MDMA forces the brain to release massive amounts of serotonin, which may induce acute psychosis and even damage neurons permanently. Regular users of Ecstasy may experience chronic panic attacks, recurring paranoid thoughts, depression and long-term memory or attention problems.
Ketamine for Treatment-Resistant Depression

A powerful anesthetic and hallucinogen, ketamine has also been used experimentally to treat addiction. In some clinical tests, ketamine reduced cravings for cocaine, enhanced mood and decreased depression, although this type of treatment is still in the early stages. Researchers speculate that ketamine’s ability to help an addict involves promoting the development of new neurons and inhibiting the reconsolidation of memories related to drug-taking activities.
At FHE Health, we use ketamine to treat depression, and while it isn’t effective in every case, we’ve successfully helped many people whose symptoms were resistant to other treatments and who felt they were running out of options. Ketamine treatment for depression has relatively few side effects, especially when the treatment is delivered in a controlled environment under medical supervision.
Ayahuasca
Ayahuasca is a tea made from the stalks of the Banisteriopsis Caapi vine and the leaves of a shrub called Psychotria Viridis. These plants are native to South America and traditionally found in the Amazon rainforest. When the plants are combined and brewed, they produce a powerful hallucinogenic drug that’s used by many tribes as part of spiritual or religious ceremonies.
Ingesting the drug can cause euphoria and hallucinations, but it may also cause nausea, vomiting, sweating and feelings of terror or paranoia. Some people believe that going on a spiritual journey through ayahuasca can help beat addiction. Research into this is limited; however, some small studies do suggest that traditional Amazonian medicine may help those other treatment options have failed. One major challenge is that the effects of ayahuasca are unpredictable, and it’s difficult to manage the dosage, especially when the drug is taken in the traditional way as a brewed drink.
Psilocybin Dosing for Alcoholism and Addiction
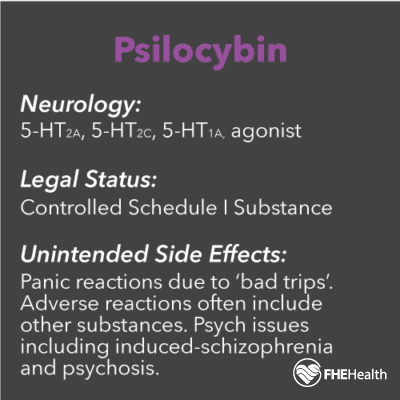
A naturally occurring chemical compound found in several hundred species of mushrooms, psilocybin is converted in the body to a hallucinogenic substance called psilocin. It produces mind-altering effects similar to mescaline, LSD and Ecstasy.
A small amount of research exists involving the use of psilocybin to treat alcoholism. The short-term results were promising, although it’s unclear whether those who changed their drinking habits following psilocybin administration maintained the positive changes in the long term.
Another important factor to consider is that experiments with psilocybin for the treatment of addiction are done under controlled conditions and medical supervision to avoid subjects suffering serious adverse effects. Taking psilocybin is known to potentially cause severe panic attacks requiring hospitalization, as well as agitation, confusion, episodes of self-injury and psychotic episodes.
Ibogaine Treatment for Addiction and PTSD
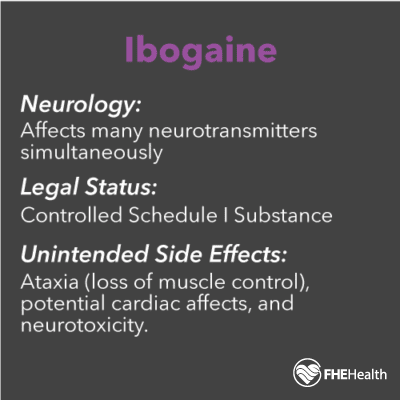
An alkaloid isolated from the bark of a West Central African tree, ibogaine is a ritual hallucinogen used by Africans that’s seriously being studied as a component of domestic addiction treatment programs. There’s also growing interest in the use of ibogaine for PTSD. It’s thought that ibogaine can help normalize or reset neuroadaptations, reducing dependence on addictive drugs. However, the way ibogaine therapy reduces cravings is unknown.
There are major safety issues with ibogaine — specifically, its potential to damage neurons and the cardiovascular system. The brain area negatively impacted by this substance is the cerebellum, which controls movement, helps regulate pleasure and fear and is involved somewhat in language, attention and cognition.
Ibogaine can also cause bradycardia and other forms of arrhythmia, which can be fatal. One challenge is that the use of ibogaine for addiction treatment in uncontrolled, nonclinical settings makes it difficult to evaluate the exact cause of these deaths. Consequently, the majority of addiction psychologists and psychiatrists consider ibogaine an experimental treatment requiring much more research before it can be legally approved to treat substance addictions.
However, experiments into treating veterans with traumatic brain injuries and comorbid issues, such as post-traumatic stress disorder, depression and anxiety, using a combination of ibogaine and magnesium have shown promising results. It’s thought that the use of magnesium can mitigate the cardiac risk associated with ibogaine.
FHE Health Believes in Evidence-Based, Safe Treatment for Addictions
While many treatment centers focus on treating only the addiction, FHE Health focuses on healing the body, mind and inner self. At our recovery center, patients address the underlying issues of their addiction while gaining the coping and life skills tools they need to achieve the goal of sobriety and take control of their lives again.
If you’re searching for addiction help for yourself or someone you care about, remember that few treatment centers set their standards as high as we do. Call FHE Health today to learn more about our outstanding treatment programs or talk to our admissions team in confidence.






