Updated on March 18, 2021
“Mush brain,” “mush brain alcohol” and “wet brain” are unfamiliar terms to many people. While unsettling, the words are memorable short descriptors of a disease that can affect long-term alcoholics at some point in the trajectory of their addiction. The disease is called Wernicke-Korsakoff syndrome.
What You Should Know About Wernicke-Korsakoff Syndrome
Wernicke-Korsakoff syndrome (wet brain syndrome) is a neurological condition that consists of two different syndromes. Both involve a severe vitamin B1 (thiamine) deficiency.
Wernicke’s encephalopathy affects the individual’s nervous system. Korsakoff syndrome is considered a cognitive disorder. A combination of Wernicke encephalopathy and Korsakoff syndrome is diagnosed in alcoholics suffering a long-term, vitamin B deficiency and alcohol-induced damage to their brain.
Thiamine (B1) and Alcoholism
Alcohol inhibits the absorption of thiamine in the intestines, the primary part of the body where nutrients enter the bloodstream. An essential nutrient, vitamin B1 must be obtained by eating food containing thiamine, such as poultry, peas, brown rice, whole grains, and bread.
Thiamine is mostly found in the brain, kidneys, liver, and heart. This explains why individuals with wet brain syndrome have a variety of serious medical issues. Heart and nervous system cells are extremely sensitive to a thiamine deficiency. Congestive heart failure and extensive cognitive impairment (“mush brain”) are often the cause of alcoholics requiring long-term hospitalization or nursing home care.
Symptoms of Wernicke Encephalopathy
Wet brain syndrome consists of the severe, short-lived Wernicke encephalopathy symptoms and the more debilitating, longer-lasting Korsakoff syndrome symptoms. Wernicke encephalopathy is specifically caused by a thiamine deficiency. Symptoms can commence quickly.
Early signs of Wernicke encephalopathy include:
- The progressive loss of appetite/dramatic weight loss over one year
- Drowsiness, fatigue, lethargy
- Craving carbohydrates/eating nothing but sugary, high-fat foods
- Regularly vomiting for more than 30 days
- Anemia, dehydration, and other medical problems due to malnutrition
- Worsening memory loss/difficulty thinking clearly
Later stage symptoms of Wernicke encephalopathy involve:
- Mental confusion/inability to comprehend conversations
- Ataxia (loss of muscle strength and coordination)
- Leg tremors
- Nystagmus (rapid back-and-forth eye movement)
- Jerky eye movements, problems with double vision
- Drooping eyelids
- Inability to walk or movement difficulties
- Problems with balance, such as trouble standing up
- Lowered blood pressure upon standing
- Rapid heartbeat
- Weakness in the arms and legs
Most people with Wernicke encephalopathy experience a progressive worsening of symptoms. Treatment with injections of thiamine should be started as soon as possible. Other treatment includes proper hydration and nutrition. Medications may be prescribed. After symptoms have worsened, individuals with Wernicke encephalopathy will need supportive care in long-term care facilities specifically designed to help people with severe dementia.
Symptoms of Korsakoff Syndrome
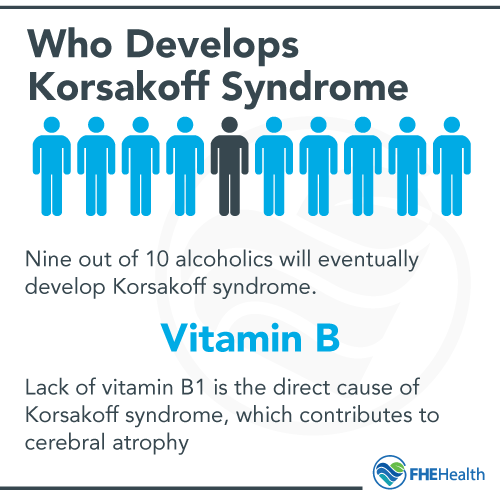
Nine out of 10 alcoholics (mostly men between 45 and 65 years of age) will eventually develop Korsakoff syndrome, also called Korsakoff psychosis. This is a neuropsychiatric condition characterized by amnesia and behavioral abnormalities.
Causes of Korsakoff Psychosis
This severe psychosis is caused by a deficiency in thiamine. Amnesia is typically found in people with alcohol use disorder (AUD). However, it’s caused more by their poor diets than their alcoholic consumption. Therefore, people with other medical conditions can develop Korsakoff psychosis if they have an insufficient intake of thiamine.
Cognitive Impairment Problems with Korsakoff Psychosis
A lack of vitamin B1 (thiamine) is the direct cause of Korsakoff syndrome, which contributes to cerebral atrophy and the following cognitive problems:
- Anterograde Amnesia – Also called proactive amnesia, anterograde amnesia is the inability to make new memories. It is nearly impossible for people with Korsakoff syndrome to learn and retain new information. This refers to short-term memory processing.
- Retrograde Amnesia – With this type of amnesia, people with Korsakoff psychosis forget what they said or did within an hour or so after it occurred. It also means forgetting what someone knew before their amnesia set in. Symptoms may start to occur after memory loss has begun. This is irreversible, so the goal is prevention before amnesia happens.
- Confabulating, or making up things they cannot remember but insist happened. To confabulate does not, however, mean telling a lie. Korsakoff syndrome patients believe the explanations their brains invent.
- Experiencing auditory or visual hallucinations that may persist or randomly come and go.
Korsakoff syndrome should not be confused with Alzheimer’s disease. Although these two disorders share similarities involving memory and cognitive problems, people with early to moderate stage Korsakoff syndrome can still socialize and perform basic daily tasks. It is possible to have a normal conversation with someone with Korsakoff syndrome, but that person will probably not remember the conversation an hour or two later.
Recognizing Signs of Wernicke-Korsakoff Syndrome
In most cases, symptoms of Korsakoff syndrome are preceded by symptoms of Wernicke encephalopathy. When an alcoholic suffers an acute lack of vitamin B1 too rapidly, the onset of Wernicke encephalopathy may be severe enough to demand emergency medical attention. In addition to muscle weakness, extreme confusion and agitation, the person will likely require treatment for tachycardia (abnormally rapid heartbeat), postural hypotension (extremely low blood pressure when standing up from a sitting position) and loss of consciousness.
Do All Alcoholics Develop Wernicke-Korsakoff Syndrome?
If someone develops a drinking problem, seeks treatment within a few years of the onset of their alcoholism, and remains sober, chances are they’re not at risk for developing Wernicke-Korsakoff syndrome. On the other hand, chronic alcoholics, or those who consistently drink for many years and never enter alcohol rehab, are likely to suffer symptoms of Wernicke-Korsakoff syndrome.
Alcohol dementia can strike men and women as young as 30. However, it’s more commonly seen in older people.
Besides, the onset of Wernicke-Korsakoff syndrome and symptom severity is not considered to be a direct relation to how much or what kind of alcohol a person drinks over their lifetime. Genetics, preexisting conditions, and other factors help determine whether an alcoholic eventually develops this mush brain disease.
Although Wernicke-Korsakoff syndrome has a low prevalence of between 0.4 percent and nearly 3 percent, doctors believe this disease is frequently misdiagnosed or underreported. Studies have found that about four out of every 100 cases of Wernicke-Korsakoff syndrome were missed because the brain was not microscopically examined during an autopsy. Other studies discovered that between 22 percent and 29 percent of people diagnosed with general dementia were alcoholics.
What Is the Standard Treatment for Wernicke-Korsakoff Syndrome?
The treatment goal for Wernicke-Korsakoff Syndrome is to improve symptoms and delay the disease progression. Following medical detoxification and complete physical and mental evaluation, people with wet brain disease receive intravenous administration of thiamine, magnesium, or both. Most patients see improvement in their physical and mush brain cognitive functioning within several weeks. Once they’ve been discharged from the hospital, patients should continue the regimen of taking oral thiamine and other recommended vitamin supplements.
There is no current cure for the Wernicke-Korsakoff syndrome. Medical experts say the best treatment for living with this disease is to stay sober, eat healthily and receive the most appropriate support for their ongoing cognitive and physical needs.
Living with Wernicke-Korsakoff Syndrome
How life with Wernicke-Korsakoff syndrome continues depends on how severely someone is affected by the disease and wet brain symptoms. Importantly, they may be able to live on their own with assistance from their caregivers or home health aides. Also, they would benefit from receiving outpatient treatment that involves individual and group counseling services, life skills training and learning effective relapse prevention techniques from addiction counselors.
When a person is in the final stages of a wet brain, they will need 24/7 nursing care. Alcohol is a neurotoxin that shrinks the brain (a phenomenon known as “cerebral atrophy”) and slowly destroys the frontal lobe, cerebellum and limbic system. In many ways, end-stage alcohol dementia resembles end-stage Alzheimer’s disease and requires the same level of intensive medical support.
Seeking Help for Wernicke-Korsakoff Syndrome
Wernicke-Korsakoff Syndrome is not a death sentence. It is a serious disease that requires professional treatment. For those who’ve been diagnosed with the syndrome, the goal is improving symptoms and delaying disease progression.
What about heavy drinkers and those concerned about the physical and mental issues they’re beginning to experience from alcohol consumption? They can benefit from getting help before the syndrome sets in. There’s no certainty that an alcoholic will develop Wernicke-Korsakoff syndrome. It is, however, more likely to occur with long-term alcoholics who’ve failed to get treatment for their addiction.
What can treatment for alcohol abuse and addiction do to stave off Wernicke-Korsakoff syndrome? The adage of “sooner than later” seems to apply here. The earlier someone seeks help for their drinking, the quicker they can resume a normal life. They’ll also have a greater likelihood of avoiding serious medical and psychological complications from alcoholism. This includes helping to prevent the development of Wernicke-Korsakoff syndrome. After all, no one wants to suffer from mush brain or go through lingering mush brain alcohol effects.
To get started:
- Admit there’s a problem with drinking.
- Learn more about how alcohol and drug treatment can help.
- Ask about treatment programs for drug and alcohol abuse.
- Commit to entering treatment and stick with it to completion.
- Join a support group to help reinforce a commitment to sobriety.
- If Wernicke-Korsakoff has been diagnosed, seek help from outpatient treatment centers.
- If long-term care is necessary, investigate available round-the-clock nursing care.
For more information about Wernicke-Korsakoff syndrome, mush brain, alcoholic wet brain and our comprehensive alcohol abuse treatment programs, call FHE Health today at (833) 596-3502. Day or night, our team of caring counselors is waiting to receive your call.