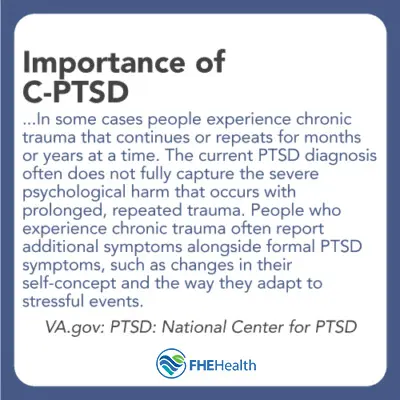
Complex post-traumatic stress disorder, or “complex PTSD” or “C-PTSD,” is a response to distressing events that occur either repeatedly or over a prolonged period. This “prolonged trauma” can significantly affect a person’s health, relationships, and quality of life.
Greater awareness of prolonged trauma and C-PTSD can relieve this burden, not just on individuals and families but on society at large. This article will explore what prolonged trauma is and describe C-PTSD in greater detail, including its symptoms, causes, diagnosis, and treatment.
Understanding Prolonged Trauma
Prolonged trauma, as its name implies, is an accumulation of traumatic experiences rather than a one-time event. Often, it entails actual or metaphorical captivity. Examples of these situations, which are also risk factors for C-PTSD, include:
- domestic violence
- childhood neglect or abuse
- sexual, psychological, and/or physical abuse
- active combat
- kidnapping
- imprisonment (in a concentration camp as a prisoner of war or a victim of human trafficking)
These experiences can leave an enormous and enduring mark in more than one way. The health impact alone can be devastating. Those with a history of prolonged trauma are at higher risk of substance use and mental health disorders (in addition to C-PTSD). They are also more susceptible to cardiovascular disease and a wide range of other issues, such as arthritis, diabetes, chronic pain, and digestive disorders.
What is the Difference Between PTSD and C-PTSD?
It is not uncommon for people to lump symptoms of any traumatic event or events under the same term, “post-traumatic stress disorder” (PTSD). This can be misleading, however, because PTSD only describes symptoms that can emerge after a single traumatic event that is no longer occurring. Dr. Beau A. Nelson, DBH, L
CSW, Chief Clinical Officer at FHE Health, explained why this distinction is important:
It is crucial to understand the differences between a single occurrence traumatic event or multiple traumatic exposures. This can help in diagnosing and treating the issues a patient is experiencing … I encourage patients to fully disclose, even if they think something is small, but still on their mind sometime later
Key Differences Between PTSD and C-PTSD
There are other key differences between PTSD and C-PTSD. PTSD is an anxiety disorder that some people experience after seeing or living through a traumatic event. Fear is a natural response to danger, and in extreme cases, it can trigger changes in the body to prepare it to either face the danger or avoid it. This “fight-or-flight” response is a normal, healthy reaction that is intended to help spare a person from harm.
PTSD
When these symptoms persist weeks after the danger is gone or appear months or years later, a diagnosis of PTSD may be at play. Symptoms can vary but generally involve:
- Flashbacks, distressing thoughts, or recurring dreams and/or memories (the re-experiencing of the event)
- Avoiding places, events, or things that remind them of the event
- Increased arousal and/or reactivity, such as being easy to startle, feeling tense, anxious, or irritable, trouble sleeping and/or concentrating
- Changes in mood and/or cognition like ongoing negative emotions (fear, anger, shame), exaggerated self-blame, feelings of social isolation, a loss of interest in previously enjoyable activities
C-PTSD
C-PTSD, which requires an experience of prolonged trauma, can be characterized by many of these symptoms but others as well. The following distinctive features of the diagnosis help to illustrate why C-PTSD requires a unique understanding and treatment:
- Problems of self-perception: The individual may feel extremely different from others. They may feel worthless, ashamed, or guilty.
- Difficulty regulating emotions: A person with C-PTSD may experience extreme anger, perpetual sadness, or even suicidal thoughts.
- Dynamic consciousness: Individuals with C-PTSD may re-experience trauma but also forget about these events. Their consciousness appears interrupted at times, and they feel disassociated from their body.
- Problems with relationships: People with C-PTSD often experience relationship problems because they struggle to trust. They may prefer isolation or seek out people to “rescue” them.
- Problematic perceptions: An individual with C-PTSD may also experience distorted feelings about the individual who perpetrated the trauma. They may feel fixated on the individual or filled with feelings of revenge.
These features are more closely associated with C-PTSD than PTSD because they occur with chronic trauma. Medical providers who note these symptoms in conjunction with prolonged trauma are likely to carefully consider a C-PTSD diagnosis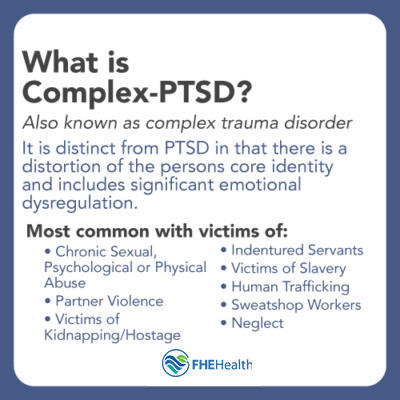
What are the Symptoms of C-PTSD?
Related to these features are the unique symptoms that differentiate C-PTSD from PTSD. An individual dealing with complex PTSD may experience specific changes in the way they perceive themselves and others. These changes may manifest as cognitive, emotional, behavioral, and/or social symptoms…
Cognitive Symptoms
- Repression of Memories: Someone with Complex PTSD may avoid thinking about people or places that are associated with the events.
- Flashbacks or Dissociation Experiences: In some cases, someone with complex PTSD may experience flashbacks that relate to memories that are beyond their control or understanding; they might respond to a specific situation instinctively because of those repressed memories and not understand their reaction.
- Forgetfulness: An individual may react or take action in times of extreme stress and not fully remember how and why they did so.
- Obsessive Thoughts: An individual may become preoccupied with the person or people who caused their trauma; with regular PTSD, they may feel a loss of power associated with that person, but C-PTSD can lead to an obsessive desire for revenge.
Emotional Symptoms
- Problems Managing Emotions: An individual with Complex PTSD may have difficulty managing their emotions. This can lead to depression, issues controlling anger, and even thoughts of suicide.
- Negative Feelings: An individual may feel helpless, detached, or guilty, or they may struggle with feeling unable to connect with others or always feeling different from those around them.
- Sense of Hopelessness: An individual may not be able to believe that people, overall, are good or enjoy positive thoughts about the future.
Social/Relationship Symptoms
- Difficulty Trusting Others: An individual may have difficulty trusting others, so they self-isolate themselves and avoid friendships and healthy relationships.
Behavioral Symptoms
- Loss of Motivation: Because someone with C-PTSD can’t maintain hope in the future, they may be unmotivated to do anything for themselves—even if they intellectually want to—today.
- Substance abuse: It’s also not uncommon for individuals with C-PTSD to turn to drugs or alcohol as a way to self-medicate. They may feel numb, out of control or unable to deal with daily life and use substances to sleep, get through the day, or push themselves out of a very tight comfort zone shell so they can function in society, at least briefly. (Self-treating C-PTSD can result in the added challenge of addiction, however.)
Symptoms of C-PTSD do often overlap with symptoms of PTSD, so their presence alone may not initially point to one diagnosis over the other. For example, someone with C-PTSD may re-experience the trauma through flashbacks or intrusive thoughts and feel routinely on edge. They may also have difficulties managing emotions, feelings of worthlessness or guilt, or suicidal thoughts. Panic attacks can occur with C-PTSD, just as they can with PTSD, but complex traumas can dig even deeper mental and emotional scars than singular traumas.
Causes of C-PTSD
Causes of C-PTSD, as mentioned above, often involve childhood abuse and neglect and long-term exposure to trauma. These situations frequently lead to other mental health issues, so it is not uncommon for a diagnosis like borderline personality disorder to occur with and contribute to C-PTSD. BPD disrupts a person’s ability to regulate their emotions and is characterized by severe mood swings, risky behaviors, relationship issues, and poor self-image.
How is C-PTSD Diagnosed?
To diagnose C-PTSD, medical caregivers will carefully evaluate the nature of the individual’s trauma as well as the age they were when they experienced the trauma. Long-term childhood trauma, in the form of neglect or abuse, increases one’s risk. C-PTSD can also develop in adulthood, however, as the result of chronic trauma.
Dr. Judith Herman of Harvard University and other professionals have called for C-PTSD to be added as a singular diagnosis to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). They base their view on evidence that prolonged traumatic experiences can lead to C-PTSD and, therefore, require specialized treatment.
Diagnostic Criteria for C-PTSD
C-PTSD is listed in the World Health Organization’s 11th revision of the International Classification of Diseases (ICD-11) but does not appear as an independent diagnosis in the DSM-5. (The DSM-5 is the American Psychiatric Association’s official textbook for diagnosing psychiatric conditions.) A subtype of PTSD, which the DSM-5 describes as “dissociative,” has many of the same symptoms of C-PTSD.
Are There Challenges in Diagnosing C-PTSD?
92 percent of people with C-PTSD also met the diagnostic criteria for PTSD in a study reported by the Department of Veterans Affairs. This finding points to one of the challenges in diagnosing C-PTSD: It can often be misdiagnosed as PTSD. Because C-PTSD is a relatively new diagnosis and does not appear in the DSM-5, not all medical professionals are aware of it.
Similarities with BPD and Bipolar Disorder
This problem of misdiagnosis extends to other conditions as well. Some of the symptoms of C-PTSD may signal borderline personality disorder (BPD) or another type of personality disorder. For example, self-image and self-worth problems can occur with both BPD and C-PTSD.
C-PTSD can also be misdiagnosed as bipolar disorder. Symptoms such as sudden mood swings, hyper-alertness, and suicidal thoughts can be present in both conditions. Unless the medical provider is well-versed in the diagnosis of PTSD and C-PTSD, a misdiagnosis might easily occur. The key to obtaining an accurate diagnosis is for patients to meet with a trauma-informed therapist or psychiatrist who is well-versed in the diagnosis and treatment of PTSD and C-PTSD.
Symptom Overlap with ADHD
C-PTSD and ADHD share some symptom overlap. For example, the hyper-focus associated with ADHD can resemble the hyper-vigilance associated with C-PTSD. The two conditions also share these symptoms: forgetfulness, difficulty controlling impulses, difficulty with emotional regulation, struggles with task switching, sleep disturbances, increased risk of substance abuse, sensitivity to sensory disturbance, and concentration problems.
To further complicate the diagnostic process, these two disorders can co-exist so that a person may be diagnosed with both conditions. Researchers have said that someone with ADHD may be more vulnerable to developing PTSD or C-PTSD. Conversely, someone who is predisposed to ADHD might develop it after experiencing a traumatic event.
Impact of Childhood Trauma on Brain Development
It’s important to note that many people who have been diagnosed with C-PTSD experienced chronic trauma as a child. A child’s brain will adapt to its environment because it’s neuroplastic, which is to say that it is still changeable in its development stage and, therefore, quite vulnerable to trauma. The symptoms that C-PTSD children experience look very much like ADHD, which makes it challenging for physicians to diagnose. Moreover, doctors might overlook a patient’s ADHD if they experienced serious trauma as a child.
These challenges in diagnosing C-PTSD reinforce the importance of seeing a specialist who can provide a professional evaluation and assessment. Mental health providers who have experience treating PTSD and C-PTSD, as well as other mental health conditions, will be better positioned to make an accurate diagnosis.
What are the Treatments for C-PTSD?
Treatment for C-PTSD may involve one or more trauma-focused therapies. Prolonged Exposure (PE), Cognitive Processing Therapy (CPT) and Eye Movement Desensitization and Reprocessing (EMDR) have been the most effective of these therapies in clinical trials. Individual psychotherapy can also help someone become more comfortable talking about their experience of prolonged trauma in a safe, supportive environment and develop tools for coping with C-PTSD in their daily life.
The root causes and triggers of C-PTSD will differ between individuals. An effective treatment plan will address these individualized causes and triggers and may include the following treatment options:
- Medication and medication management for mental health conditions that arise from true chemical imbalances or biological causes.
- Neurotherapy helps to retrain the brain to respond in certain ways to triggers. In the case of C-PTSD, Neurotherapy may help an individual retrain their mind to react without a panic attack or more calmly remember and process factors about their traumas.
- Group therapy lets participants learn about others’ journeys through trauma and understand that they are not alone in their own walk.
- Holistic approaches such as mindfulness meditation and yoga help calm the nervous system, increase mind-body awareness and build stress resilience, among other benefits.
- Recreational and other types of therapies help to strengthen healthier coping mechanisms so the individual can turn to self-care, therapy, support structures, and other positive answers instead of drugs or alcohol to deal with C-PTSD.
Is It Possible to Live With C-PTSD?
Living with C-PTSD can be challenging, especially if it is untreated. Its impact on daily life and functioning can be severe or worsen over time, in some cases leading to suicide.
C-PTSD can be hard to recover from completely, but treatment has helped many people achieve significant relief from their symptoms, as well as more peace of mind and a better quality of life. Group and individual therapy can help people develop new coping tools for managing their symptoms. A good self-care plan that includes regular exercise and a strong support network can boost overall health and mental and emotional resilience.
Conclusion
C-PTSD is a unique condition with its own set of symptoms, but it remains much less known than PTSD. This reality can contribute to the stigma and make it hard for people who suffer from C-PTSD to believe they are not alone or that healing is possible. That can change, though, with more public awareness about the disorder, its causes, risk factors, symptoms, and treatments.
Today, there are many resources for those facing this disorder. If you’re dealing with C-PTSD, you don’t have to face it alone. Contact FHE Health today to learn more about your treatment options.






