Prednisone is a corticosteroid, commonly called a steroid, that closely resembles the natural steroid hormone cortisol. It suppresses the body’s natural immune response to reduce inflammation, arthritis pain and the effects of a range of conditions. It’s prescribed to treat or lessen the discomfort associated with allergies, autoimmune disorders, cancer and more.
When an individual takes prednisone for an extended period of time, their body starts to become accustomed to the increased levels of cortisol. This means that when they stop taking prednisone, their body experiences a sudden drop in cortisol and is unprepared to regulate various processes at this lower level.
Suddenly going off of prednisone can potentially cause uncomfortable withdrawal symptoms. Knowing what to expect from these symptoms and identifying strategies for avoiding them can help individuals prevent complications
Understanding Prednisone Withdrawal Syndrome
Prednisone Withdrawal Syndrome often brings uncomfortable symptoms, making it difficult for some to stop taking the medication. Understanding the causes, symptoms and risk factors of PWS can help individuals manage the transition off this medication safely.
What is Prednisone Withdrawal Syndrome?
As is the case with most medications, the longer someone takes prednisone, the harder it is for their body to adjust to not having it. Due to the chronic nature of the conditions this medication is prescribed for, it’s fairly common for individuals to take prednisone for an extended period of time. When this happens, the body starts to become accustomed to the increased levels of cortisol. This means that when the user stops taking prednisone, the body experiences a sudden drop in cortisol and is unprepared to regulate various processes at this lower level.
Some of the most common withdrawal symptoms include:
- Mood instability
- Weakness
- Severe fatigue
- Body aches and joint pain
- Dizziness
- Light-headedness
- Appetite fluctuations
- Nausea and vomiting
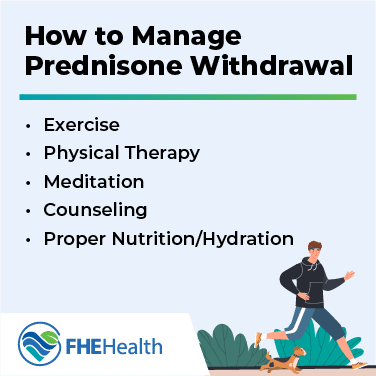
In most cases, these prednisone withdrawal symptoms last one to two days after stopping prednisone, but they can be alarming if you’re not expecting them. And, when your body is out of rhythm, it can have a larger effect on your physical and mental health than you may realize.