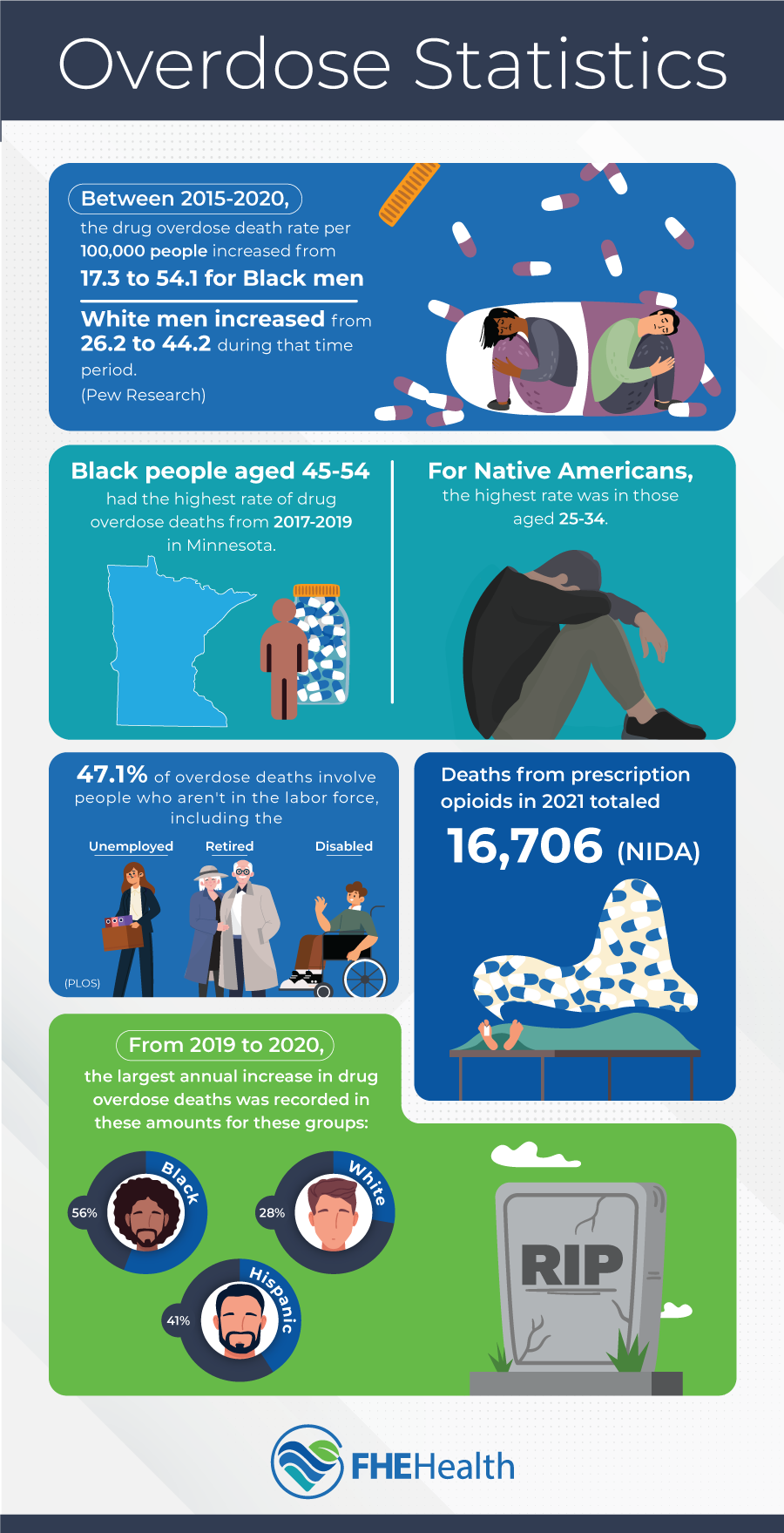
Every year in the United States, more than 100,000 people lose their lives to drug overdose. While a shocking 16,706 deaths in 2021 were directly linked to legal, prescribed medications — specifically opioids — drug overdose death rates encompass more than just those with a legal prescription. These stark overdose statistics highlight a critical public health issue.
The Opioid Crisis: Understanding the Scope of the Overdose Epidemic
Did you know that in 2012, during the peak of the opioid crisis, doctors and other medical professionals were prescribing 81.3 opioid prescriptions per 100 people nationwide? While that number dropped to a much more moderate (though still quite high) 43.3 per 100 in 2020, some specific counties had prescribing rates as much as nine times higher than the average.
With so many opioids legally accessible and obtainable, it’s no surprise that the overdose epidemic grew by leaps and bounds during this period. Even when opioids were less readily accessible, many of those who already had an addiction continued to seek out drugs afterward, though the choice of drug might change depending on the availability. For example, those who were addicted to opioids might seek out heroin or other drugs available on the street.
Demographic Disparities: Examining How Overdose Rates Vary Across Different Groups
Overdose death rates vary depending on demographics and the specific drug. Overdose statistics show that overdose rates by race are broken down into three broad categories of Black (non-Hispanic), Hispanic, and White (non-Hispanic). White non-Hispanics have the highest rate of deaths when comparing drug overdose by ethnicity, but Black non-Hispanics saw the largest single-year increase between 2019 and 2020, with a 56% increase.
Indigenous peoples also saw a substantial increase in the number of overdose deaths, with a 39% increase among American Indians and Alaskan Natives, clearly illustrating the scope of the opioid crisis by race. It’s important to note that regardless of demographic, most of those who died as a result of an overdose had no history of treatment for a substance use disorder. While lack of health insurance may have accounted for some of these deaths, many may have avoided treatment options that were available to them due to societal stigma or dosing errors that were sudden and unexpected.
Most overdose deaths involve a type of opioid, with more than 70,000 attributed to some form of synthetic opioid each year. During March to August in 2021, Black men are estimated to be the group with the largest number of opioid-related deaths, once adjusted for population. Across all demographics, drug overdose continues to be the most common cause of death for injury-related incidents.
Age and Gender Factors: Analyzing Overdose Statistics Among Various Age and Gender Categories
Age and gender also play an important role in determining risk factors for overdose deaths. The age group with the highest risk of a preventable overdose death is those aged 35–44. Overdose statistics reveal that out of all overdose deaths, 71% occur among those aged 25–54. Children under age 15 rarely die from an overdose, but those 55 and over are climbing quickly, according to the National Safety Council.
Men are substantially more likely to die from an overdose, but that may be due to the simple fact that men are also twice as likely to use illicit drugs or over-consume alcohol. Men are also four times more likely to commit suicide, and most suicides also include some substance use. Ultimately, more men than women wind up in emergency rooms for overdoses, and more men die as a result of their drug use habits.
Socioeconomic Influence: Exploring the Impact of Socioeconomic Factors on Overdose Rates
Many socioeconomic factors contribute to overdose death rates, ranging from total household income to where you live and your insurance status. Some of the factors most likely to impact your risk of an overdose include poverty level, rural versus urban living and employment status.
Nearly half (47.1%) of all overdose deaths are attributed to those not in the labor force. This includes those who are retired and those who don’t work due to disabilities or other factors. Depression and societal judgments toward those who don’t work may play a role in these deaths, along with other mental illnesses and contributing factors.
Those earning more than 500% above the poverty line are at substantially reduced risk of opioid overdose. This likely includes the higher risk associated with a lack of insurance. Those without insurance are less likely to seek treatment early during an overdose and less likely to seek any type of substance use treatment overall, due to cost concerns.
In general, living in more densely populated areas increases the risk of a drug overdose death due to two main factors: availability of drugs and health care. When a hospital is more than 20 minutes away by car, it makes it more difficult to seek treatment in a timely fashion. The longer the delay between the overdose and treatment, the more likely a patient is to die from complications related to an overdose.
Implications for Action: Addressing Demographic-Specific Overdose Trends in Prevention Efforts
Knowing what groups are most likely to face an overdose helps governments and private organizations attempting to combat this epidemic. If you know who’s most at risk, you can work to provide preventive care and make health care as accessible as possible.
Programs that provide subsidized substance use disorder treatment are important when trying to lower the death toll from illicit drugs and alcohol, but they work best when information is made available to the right group of people. The highest-risk groups tend to be adult men under the age of 55, so placing advertisements in areas most likely to reach this group is important.
The more you know about which groups are likely to struggle with substance use, the more help you can provide within your own family and friend groups.
Take the First Step Towards Recovery
If you or someone you know is struggling with addiction, reach out to FHE Health today. Our compassionate counselors are always available to help you schedule treatment.