Transplants involving those with a past of substance abuse has led to new opportunities but also new questions.
One of the tragic outcomes of the opioid overdose crisis is the availability of more organs for those waiting for life-saving transplants. Though a very sad consequence of this crisis, many younger people are dying, and their organs may be healthy enough to donate.
On the other side of the coin, drug use can lead to addicts needing transplants when organs begin to fail due to substance abuse. Here’s a closer look at organ donation and addiction.
Know the Data About Organ Transplants
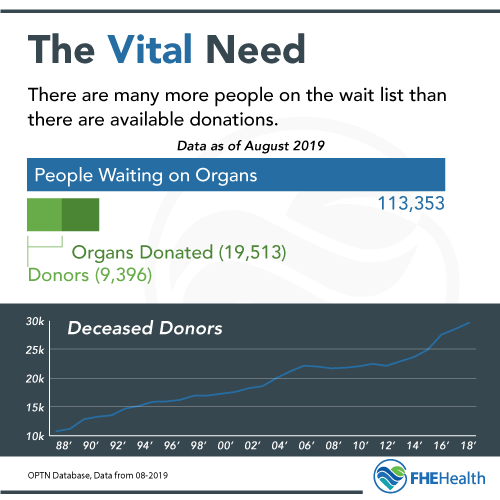 The United Network for Organ Sharing reports that 113,353 people are waiting for a lifesaving organ as of July 2019. From January through June 2019, there were 19,513 transplants in the United States from 9,396 donors.
The United Network for Organ Sharing reports that 113,353 people are waiting for a lifesaving organ as of July 2019. From January through June 2019, there were 19,513 transplants in the United States from 9,396 donors.
The numbers are clear. There are many more people on the waiting list than there are available donors.
In the last few years, the number of available donors has grown. Unfortunately, this is a direct result of the number of people dying from opioid overdoses and complications. Though these hearts, kidneys, livers and other organs are considered a higher risk than those from an otherwise healthy donor, they may still be very viable organs.
Because these organs come from a donor with a history of drug abuse, some recipients have elected to turn them down. For some, the risk of complications due to the damage drugs cause to the organs is just too high.
There is also a higher risk that the organs from drug users have hidden illnesses such as hepatitis or HIV. While there are certainly policies and procedures in place to screen for these factors before a transplant is complete, and most hepatitis infections are curable, this may not be enough reassurance for the person on the transplant list. Furthermore, for someone with a compromised immune system due to organ transplant medications, these diseases and associated damage can lead to complications.
How Does Drug Use Damage Organs?
Whether addicts can donate organs really depends on the condition of those organs and the person’s overall health. In living donor cases, such as kidney transplants, doctors must consider the risks to the person receiving the damaged organ. Drug users’ organs may have damage related specifically to the drugs used.
As noted by the National Institute on Drug Abuse, drug use can create a wide range of risk factors for organ health:
- Inhaled substances damage the lungs and the entire respiratory system.
- The toxins in blood from illicit substance use can damage the vascular system, even destroying tissue in the heart.
- Sharing needles can transmit HIV/AIDS or other infectious diseases.
- The work of flushing toxins out of the body can cause long-lasting damage to the kidneys and liver.
- Poor nutrition and damage to tissues can cause musculoskeletal problems.
- Those who use drugs are also at a higher risk of developing some forms of cancer, which can transfer to an organ recipient through transplant.
Not All Organs Suffer Damage
The increase in the number of organs donated by drug users who have overdosed is possible because not all organs suffer damage right away. Often, those who have been using drugs for a short time have relatively healthy organs. This may be the case in someone with a short history of drug abuse and sudden overdose.
These remain suitable for transplants. The type of drug, the amount used, the method it was taken, the overall health of the individual who has died and other factors play a role in the worthiness of the organs for transplant.
What Doctors Do to Minimize the Risks
Doctors may or may not discuss these factors with the patient prior to transplant. Due to the publicity organ recipients and the organ donor’s family often receive, we may get the perception that everyone gets to meet, but that is not always the case. Both parties must give consent to disclose this information as it is health information. Prior to a transplant, what the doctor can reveal to the recipient is basic facts about the donor and may or may not include substance abuse history. These organs can include those from living opioid users or those that become available after a person dies of an opioid overdose. If the patient does learn this information and chooses not to receive the organs, they must wait for another organ to become available.
If the recipient agrees to a higher-risk organ, they have numerous protections against the risks. Specialists perform blood tests and a significant inspection of the organ. Doctors never transplant an organ that looks unhealthy or doesn’t seem to function at 100%.
What If You’re the User Who Needs an Organ?
 There’s another side to this process. For some, years of drug abuse leads to damage to their organs.
There’s another side to this process. For some, years of drug abuse leads to damage to their organs.
Smokers’ lungs become cancer-filled. Kidneys stop working properly. Some people develop alcoholic liver disease.
They may need a transplant to overcome this damage, but are they able to obtain one? The answer depends on the specifics of your situation.
With over 100,000 people waiting for an organ, there are several standards followed that organize the priority. The main factors are the need, location, and match potential, but superseding those are that the recipients adhere to the policies of being on the list. The reason for this is very simple.
There aren’t enough available organs to meet the need. UNOS, which is the transplant organization for the entire United States, wants to ensure that the people who are most likely to thrive and do well with the organ get the opportunity to do so. A component of that is UNOS compliance requirements.
What Do You Have to Do to Get on the List?
When a substance abuser needs an organ, the first step is to prove they’re no longer using. In most cases, this means that they need to be drug-free, alcohol-free and smoke-free for six full months before UNOS allows them to be listed.
There are some situations where this may not be the case. During those six months, you need to have several screenings and blood tests, including random testing, to determine if you’re clean. If not, the six-month time frame may start over.
Your doctors can support your efforts. Medications and other treatments may help you bridge the gap between needing a transplant and getting clean. And when you are as healthy as possible heading into transplant, your chances of long-term recovery are far better than what you may expect otherwise.
Getting Clean to Get an Organ
 No matter where you are right now on your path to improving your health, drug and alcohol rehabilitation may be the first step. By working through a rehab program including detox, you may be able to prove to your doctors that you deserve the opportunity to be listed on the organ transplant list. Getting clean isn’t an option’ it’s a requirement for obtaining a new chance at life.
No matter where you are right now on your path to improving your health, drug and alcohol rehabilitation may be the first step. By working through a rehab program including detox, you may be able to prove to your doctors that you deserve the opportunity to be listed on the organ transplant list. Getting clean isn’t an option’ it’s a requirement for obtaining a new chance at life.
Getting the Care You Need at FHE Health
Find out how to enroll in detox and start on the path to a clean life to improve your health. Call our compassionate team now at (833) 596-3502 to discuss your options.






