
If you’ve ever dealt with intense muscle spasms or back pain, your doctor may have prescribed a muscle relaxer. Designed to deliver short-term pain relief, they’re often used to treat acute pain, muscle spasms and certain neurological conditions. While they can be effective when used as directed, some patients may wonder: Are muscle relaxers addictive?
The answer depends on the type of muscle relaxer, duration of use and individual risk factors. In this article, we examine how muscle relaxers work, their potential for misuse and the health risks that can arise from abuse or long-term dependence.
What Are Muscle Relaxers, and Why Are They Prescribed?
When it comes to pain, many people turn to over-the-counter drugs. Although OTC medications help temporarily block pain signals, they don’t address the root cause of muscle spasms. That’s where muscle relaxers come in.
Muscle relaxers are prescription medications used to relieve spasms, stiffness or pain caused by conditions including:
- Back injuries
- Brain or head injuries
- Multiple sclerosis
- Stroke
They’re often used alongside other treatments, such as physical therapy.
How Do Muscle Relaxers Work?
Muscle relaxers relieve pain and discomfort by reducing involuntary muscle activity. However, not all muscle issues are the same — and neither are the medications used to treat them. Muscle relaxers are generally categorized in two ways: by how they work (centrally acting vs. direct-acting) and by what they treat (antispasmodic vs. antispastic).
Antispasmodics treat muscle spasms — sudden, involuntary contractions caused by injury, strain or tension. Rather than targeting the muscles directly, these drugs reduce nerve signals in the brain or spinal cord that lead to spasms. Most centrally acting muscle relaxers, such as cyclobenzaprine, tizanidine and methocarbamol, fall into this category.
Antispastics, on the other hand, treat muscle spasticity — a condition in which muscles remain continuously tight due to nerve damage or neurological disorders, such as multiple sclerosis or cerebral palsy. Spasticity differs from spasms in that it’s more sustained and often linked to central nervous system dysfunction. Some antispastics, such as baclofen, are centrally acting, while others, including dantrolene, are direct-acting.
Are Muscle Relaxers Addictive?
Muscle relaxers are usually safe when used as prescribed. If misused, however, dependency can occur. People may misuse muscle relaxers for the following effects:
- Euphoria or mild “high”
- Sedation or deep relaxation
- Muscle numbness or reduced tension
- Drowsiness or sleep aid effects
Due to the euphoric sensation associated with these drugs, you might question: Do muscle relaxers make you high? The answer is yes — if they’re being misused. Centrally acting muscle relaxants, such as cyclobenzaprine or carisoprodol, can cause a sense of calm or mild intoxication, especially when taken in high doses or combined with other substances such as alcohol or opioids.
Over time, misuse may lead to psychological dependence, where individuals feel they need the drug to relax or sleep. Physical dependence can also occur, particularly with drugs that act on the central nervous system. Stopping abruptly may lead to withdrawal symptoms, including anxiety, tremors or rebound muscle spasms.
Federal data shows that misuse remains a common concern. According to the Drug Enforcement Administration, cyclobenzaprine — a commonly prescribed muscle relaxer — was identified in over 450 drug-related forensic reports each year from 2021 through 2023. While this doesn’t confirm widespread addiction, it highlights ongoing patterns of nonmedical use.
Short- and Long-Term Health Risks of Misuse
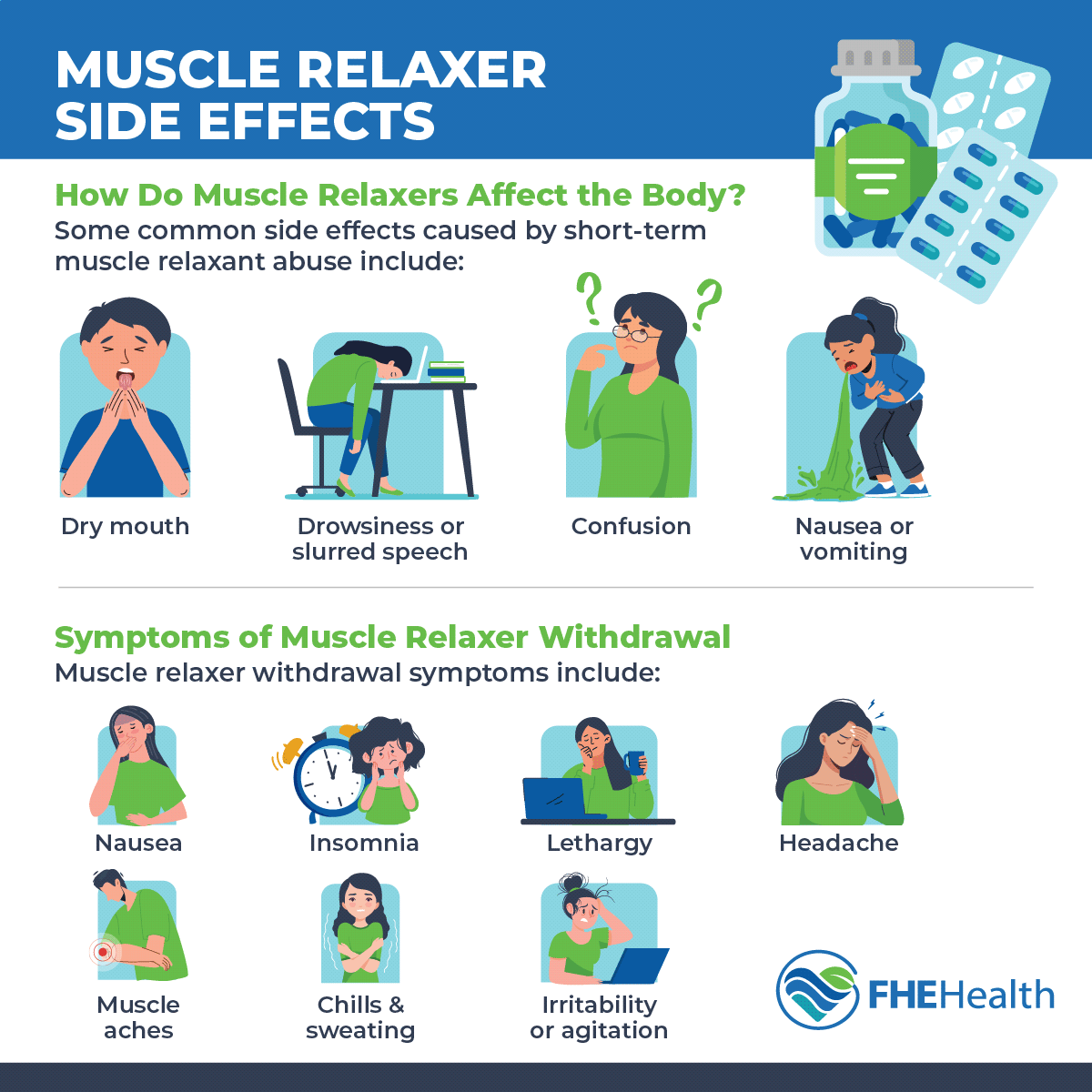
Misusing muscle relaxers — whether by taking higher doses, combining them with other substances or using them without a prescription — can lead to serious short-term and long-term health consequences.
Short-term risks include:
- Excessive sedation. Muscle relaxers depress activity in the central nervous system, which can cause extreme drowsiness, lethargy or fainting.
- Respiratory depression. When combined with alcohol, opioids or other sedatives, muscle relaxers can slow breathing to dangerous levels.
- Reduced motor control. These medications can impair coordination and balance, making everyday tasks such as walking or driving hazardous.
- Dizziness. Changes in blood pressure and slowed brain activity may cause lightheadedness or unsteadiness, increasing the risk of falls or accidents.
- Blurry vision. Some muscle relaxers interfere with nerve signaling related to vision, resulting in temporary visual disturbances.
Long-term risks include:
- Physical dependence. With repeated misuse, the body can become accustomed to the drug, requiring higher doses to achieve the same effects.
- Withdrawal symptoms. Suddenly discontinuing muscle relaxers after prolonged use can cause symptoms such as anxiety, irritability, tremors, insomnia or muscle pain.
- Cognitive impairment. Long-term use may negatively affect memory, focus and decision-making.
- Liver damage. Certain muscle relaxers, particularly those metabolized by the liver, may contribute to liver strain or injury when taken in excessive doses or over extended periods.
If too many muscle relaxers are ingested, there’s a risk of overdose. An overdose can lead to loss of consciousness, coma or (in severe cases) death.
Treatment Options for Dependence and Addiction
Dealing with a dependency on muscle relaxers isn’t easy. Fortunately, treatment is available. Recovery often requires a combination of medical supervision, behavioral support and long-term care planning.
Medical detox is typically the first step. This involves gradually tapering the medication to minimize withdrawal effects. A health care provider supervises the process to help prevent any adverse reactions. In some cases, short-term use of alternative medications may be prescribed to manage symptoms and reduce cravings.
Once detox is complete, it’s important to take steps to prevent future dependency. Approaches such as cognitive behavioral therapy can help individuals develop healthier coping mechanisms and identify triggers, reducing the risk of relapse. Additional support options include:
- Outpatient counseling or addiction therapy. These programs offer flexibility while still providing structure and accountability.
- Inpatient treatment. For more severe cases, residential programs offer a controlled environment with round-the-clock care.
- Support groups. Peer-based recovery communities can provide ongoing encouragement and connection.
- Aftercare planning. Continued check-ins with health care providers help reinforce progress and prevent relapse.
If you or a loved one is struggling with muscle relaxer dependency, you’re not alone. Speaking to a mental health professional who understands your condition is critical. Through a combination of talk therapy and medical treatment, you can overcome dependency and regain control of your life.
FHE Can Help
At FHE Health, we recognize the unique physical and mental challenges that come with muscle relaxer misuse. We offer a thorough diagnosis process as well as a wide range of treatments geared toward improving quality of life. Contact us at FHE to learn more about our programs and how we can help you.






