
The intensities of war, demand for mental and physical toughness, and separation from family make military veterans susceptible to a wide range of mental health risks. Understanding these risks and the available treatment options is crucial for the well-being of our veterans.
The Scope of Veteran Mental Health Challenges
The prevalence of mental health challenges within the military community is a significant concern. The Department of Defense Suicide Event Report revealed just how widespread military mental health challenges can be: In 2013, there were 1,080 suicide attempts and 245 suicides among active-duty service members.
A longer-ranging study released by the U.S. Department of Veterans Affairs found that, from 2008 through 2016, about 6,000 veterans committed suicide each year. That represented a roughly 26 percent increase in the suicide rate for veterans during this period. The study also noted that as many as 1 in 4 active-duty members of the Armed Forces have some signs of a mental health disorder.
Meanwhile, the RAND Center for Military Health Policy Research found that 20 percent of individuals who served in either Afghanistan or Iraq struggled with major depression or PTSD. It is clear from these statistics that there is an urgent need for accessible and effective veteran mental health care.
Treatment can begin quickly and discreetly, get started now Veterans are at risk for a variety of mental health disorders. Mental illness in the military can include: One of the most common forms of mental illness in the military occurs after traumatic events such as disasters, sexual assault, physical assault, or military combat. These events can create long-term negative thought patterns. Over time, individuals who do not manage these thoughts and feelings can develop nightmares, anger, aggressiveness, difficulty sleeping, and restlessness. Some turn to alcohol and drugs as a way to soothe their feelings. This can create co-occurring disorders where alcohol or drug abuse happens alongside one or more mental health disorders in veterans. Major depressive episodes can occur in individuals coming back from a deployment of any type, including combat. In this case, depression is not just feeling sad. It typically causes feelings of helplessness, anger, frustration, and difficulty completing daily tasks. Though less common, traumatic brain injuries due to a blow to the head can alter brain chemistry. This can go unnoticed for some time until mental health issues develop in veterans. In some, this can lead to depression-like symptoms; in others, it can cause mood swings. Many experience fatigue, headaches, memory problems, and an inability to concentrate. After deployment, many individuals may have supportive family and friends but don’t open up to them for various reasons that can further aggravate their condition: Ready to start? More questions about treatment? A significant barrier to veteran mental health care is the stigma associated with seeking help. For many, the thought of obtaining help for mental health issues seems like a failure. Some men and women leaving the military never seek help, believing they can manage it on their own because their fellow veterans seem to do so. Shame, frustration, and the compulsion to “just go on” with their lives can leave men and women unwilling to seek help but immobilized by their condition. They may also encounter demographic barriers to treatment—or false stereotypes of their demographic—that cause them to doubt whether treatment will really address their needs. They may come to believe they just need to cope on their own. Another key aspect of this stigma stems from a belief that seeking care for mental health issues could limit or otherwise negatively affect their career. Although health and mental health challenges that go untreated can impact anyone’s career, today, anyone seeking help for therapy or counseling has job protections under the law. Veterans have additional legal protections when they seek treatment for a mental health condition. Rules passed by the U.S. Department of Defense in 2014 eliminate the chance that talking to a doctor or having a diagnosis of mental illness will be career-ending. Additionally, active military and veterans seeking treatment for mental health issues do not automatically disqualify an individual from serving, ranking upwards, or obtaining long-term benefits—and it does not automatically limit security clearance. Let’s be honest: For many years, the Veterans Administration didn’t offer the quality of care required for veteran mental health issues. While programs have long been in place, many did not know about them, and long wait times to see VA doctors were common. Additionally, many believe the mental health programs offered by the VA were inadequate or inferior to programs available to others. The VA has come a long way in this regard, even if there is room for improvement. If a family member were struggling with shortness of breath, they would seek emergency care. Similarly, someone with diabetes would also get help for their condition. Like these health issues and others, veteran mental health issues demand immediate care by the right medical professionals. Like other health issues also, veteran mental health issues will only worsen if left untreated. The progression might look like outward bursts of anger that evolve into violence, spiraling mental health problems, and then a psychotic break. In some situations, an untreated case of PTSD or another mental disorder can create career problems, substance abuse, and relationship issues. In the worst-case scenario, individuals with untreated mental health conditions can lash out with violence towards others and/or attempt suicide. Access to mental health treatment has limitations. Military veterans may see the VA as their only option for care, which is no longer the case. While in the past, many men and women only had access to health care through VA offices and hospitals, veteran mental health care has expanded to provide access to a larger number of providers. Tricare coverage is now more expansive, providing a wide range of treatment options beyond the actual VA. The benefits of seeking care outside of the VA for military professionals include: Every program is different, as are everyone’s needs. With the help of a specialized treatment program, veterans may be able to find a higher quality of care. This type of care may now be available through TRICARE, the military’s insurance plan. TRICARE policyholders can seek out care through a wide range of approved facilities, including FHE Health. If you or a vet you love is battling mental health challenges, our trusted professionals at FHE Health are here to help in any way we can. Our specialized program for veterans and first responders pairs trauma-based therapies with peer support groups consisting of other members of the military and first responders. To learn more about our programs for veteran mental health, call our compassionate counselors 24/7 at (833) 596-3502. https://www.apa.org/advocacy/military-veterans/mental-health-needs.pdf https://www.mentalhealth.va.gov/docs/data-sheets/OMHSP_National_Suicide_Data_Report_2005-2016_508.pdf https://www.rand.org/pubs/research_briefs/RB9336.html We offer 100% confidential and individualized treatment Kristina Robb-Dover is a content manager and writer with extensive editing and writing experience... read moreNeed Help?
What Are Common Key Veteran’s Mental Health Risks?
Post Traumatic Stress Disorder (PTSD)
Depression
Traumatic Brain Injury
Why Are Military Veterans at Risk for Mental Health Disorders?
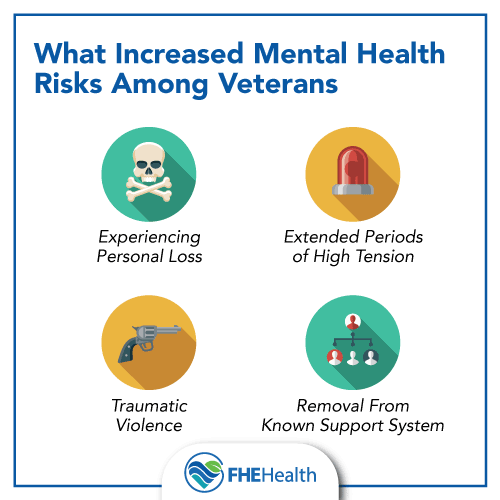 Active military and veteran’s mental health is complex since no single factor impacts every individual. For active members, especially those engaged in wartime activities, the risks of military behavioral health concerns increase significantly. Deployment alone can be a factor in the development of these challenges; however, those engaged in combat are more likely than others to experience adverse effects.
Active military and veteran’s mental health is complex since no single factor impacts every individual. For active members, especially those engaged in wartime activities, the risks of military behavioral health concerns increase significantly. Deployment alone can be a factor in the development of these challenges; however, those engaged in combat are more likely than others to experience adverse effects.
Begin your recovery today
What is the Stigma of Military and Veterans Seeking Mental Health Help?
Are There Mental Health Services at the Veterans Administration?
What Are the Dangers of Veterans Not Getting Help?
Does Veteran Mental Health Treatment Continue to Be Lacking?
Are There Benefits to Seeking Care from a Veteran Mental Health Rehabilitation Program?
 In addition to the VA, there are now many quality treatment options for vets. Many mental health treatment programs now specialize in treating veterans and their concerns through intensive inpatient and outpatient care.
In addition to the VA, there are now many quality treatment options for vets. Many mental health treatment programs now specialize in treating veterans and their concerns through intensive inpatient and outpatient care.
Get Help for Veteran Mental Health
More Questions about Treatment?
![]()
About Kristina Robb-Dover






