
Police officers expect to face challenges. They frequently encounter individuals experiencing a mental health crisis, people who may be dealing with alcoholism, addiction, delusions and hopelessness. Sometimes people are vulnerable and lack access to traditional social services. In other cases, it’s a cry for help.
However, many police officers and other first responders lack the necessary mental health training to resolve these situations effectively. In today’s world, where mental health challenges are highly complex, police departments can benefit from mental health training programs.
How Common are Encounters Between Police and the Mentally Ill?
 The primary responsibility of police officers is law enforcement. Yet the desire to keep the peace has unclear boundaries. If officers arrive on the scene and find someone in the middle of a mental health crisis, they still have to act.
The primary responsibility of police officers is law enforcement. Yet the desire to keep the peace has unclear boundaries. If officers arrive on the scene and find someone in the middle of a mental health crisis, they still have to act.
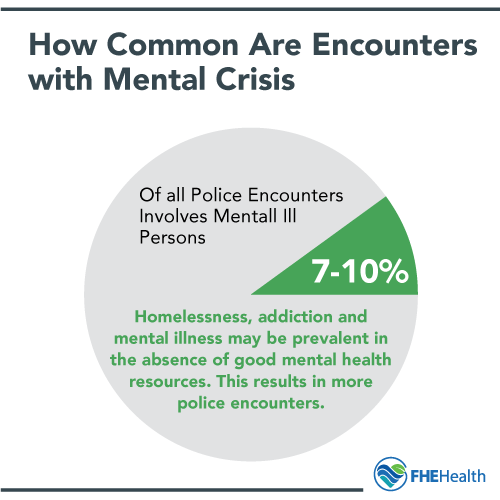
An estimated 7% to 10% of all police encounters involves mentally ill persons. Some areas, especially those in abject poverty, have a high number of people with co-occurring problems. Homelessness, addiction and mental illness may be prevalent in the absence of good mental health resources. This results in more encounters of policing the mentally ill.
While officers may be equipped to handle some situations, they aren’t a substitute for social services. Officers with limited knowledge time, and mental health training are likely to resolve a mental health crisis by detaining a disruptive person. Taking their more frequent police contact into account, it’s no wonder 2 million mentally ill people go to jail every year.
Decades after the dismantling of psychiatric institutions, police consider 2.7% to 5.9% of possible suspects as having a serious mental illness. In communities that failed to replace closed institutions with essential social services, negative encounters with law enforcement are an even greater problem.
Attempts to resolve a mental health crisis with force burdens police officers, healthcare professionals and regular citizens. Mentally ill individuals temporarily jailed for causing a disturbance will eventually be released. Without providing access to necessary care, the chances of a recurring incident are high.
What are the Challenges of Solving a Mental Health Crisis?
Police work can be a gray zone that requires both caretaking skills and the use of force. Poor areas see many calls to police for disturbances caused by someone having a mental health crisis. Officers may end up caring for those who can’t care for themselves, such as substance abusers and homeless persons. These encounters resist formal solutions.
How an officer interacts with the public is a relevant factor. Younger, less experienced officers tend to struggle with caretaking actions, opting for the use of force and detainment instead. They may also be less well-known in the community than a veteran officer who has served the same people for years. Senior officers usually have better knowledge of their patrol area, which may help them manage repeated encounters with mentally ill suspects.
Public perception and accountability is another issue. Conduct suggested by an officer’s department may not cover specific contexts with mentally ill individuals. Officers face consequences for failing to stop individuals from perpetrating criminal acts, especially if unable to initially discern their mental state.
Police also face many challenges when responding to calls about a mentally ill suspect. As a last resort, families may report a loved one who is out of control, uncooperative and potentially dangerous. Often, the family knows that police can’t force their loved one to be committed to a mental health facility voluntarily, so they call as a way to receive a break from frustrating behavior.
Police are frequently called to emergency situations with a suicidal individual. This person may even try to provoke officers into using fatal force, which is colloquially referred to as “death by cop.” In these situations, officers take on the responsibilities of psychiatrists and other social workers, despite lacking the same knowledge or experience.
It’s also common for callers to take issue with the homeless occupying public spaces, particularly if they feel threatened. Loitering in and around certain businesses like fast food restaurants or gas stations is common for those with no place to go; they are often hungry or seeking temporary shelter in inclement weather.
Furthermore, public fear of mental illness persists. Callers who have stereotypes about certain psychiatric problems, like schizophrenia and bipolar disorder, can perceive threats to their safety. Police then have to consider the well-being of both the caller, who may desire an unwarranted forceful response and the suspect.
What are the Informal Policing Approaches to the Mentally Ill?
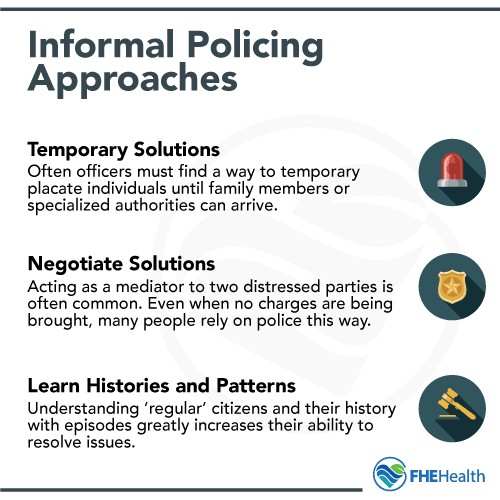 Traditional methods that focus on reducing crime and increasing clearance rates fail to adequately account for mental health needs. To deal with policing challenges the gray zone presents, many officers rely on informal methods of police work. The combination of three informal policing approaches adds a nonviolent tool to the police arsenal. This knowledge allows them to operate in variable contexts, relying on information about the community to resolve gray-zone policing problems.
Traditional methods that focus on reducing crime and increasing clearance rates fail to adequately account for mental health needs. To deal with policing challenges the gray zone presents, many officers rely on informal methods of police work. The combination of three informal policing approaches adds a nonviolent tool to the police arsenal. This knowledge allows them to operate in variable contexts, relying on information about the community to resolve gray-zone policing problems.
Officers are forced to choose temporary remedies for individuals suffering more than a mental health crisis. Situations involving the poor, sick, destitute and other chronically vulnerable people are difficult to resolve entirely. These people are unlikely to value compliance as much as those who are better off. As a result, officers offer interventions that temporarily put distressed individuals at ease.
Officers also negotiate peaceful resolutions between complainants and subjects who are mentally ill. Some cases, such as calls from hospitals and social services, involve concerns about violence and unpredictability. Others are domestic disputes that warrant social services, but officers lack the ability to involuntarily commit the call subject. However, they can still act as mediators, preventing flare-ups of larger conflicts.
Finally, officers learn local history and complaints, which helps them predict patterns of behavior and devise a soft method of interacting with mentally ill individuals. Knowing who the regulars are and what troubles they have gives officers more options in street-level situations.
How Can You Reboot the Approach to Policing the Mentally Ill?
Given the number of incidents that involve a mental health crisis, police officers can benefit from mental health awareness and training. Social workers and other medical professionals can also learn to leverage the knowledge beat officers acquire during the patrol.
Crisis Intervention Teams (CIT) are becoming the best practice for police departments in the United States and elsewhere, with over 2,700 of them implementing the approach. This method stresses reducing the use of force and connecting more individuals to appropriate mental health services. The program continues to develop variations, making it easier for departments to tailor its core methods to their local environments.
The spread of CIT in the United States suggests that more police departments are accepting mental health first aid as a serious police responsibility. By redefining their responsibilities, departments can play a vital role in assisting medical professionals.
More Resources And Support For Heroes In Law Enforcement:
- 7 Reasons First Responders Need Specialized Mental Health Treatment and Support
- In Honor of Men and Women in Blue Who Gave Their Lives – Consider the Mental Health Sacrifices That Our Police Are Making
- FHE Health Is Now the Primary Provider of Choice for National Fraternal Organization of Police
- The Real Dangers of Fentanyl Exposure for First Responders
- First Responder Mental Health at Heart of New Partnership






