If you’re among the estimated 50 million Americans suffering from chronic pain (according to the Centers for Disease Control and Prevention (CDC)), you undoubtedly yearn for an effective way to be pain-free. Among the many choices for pain relief treatment, meloxicam is a prescription-only medication that provides clinically proven relief from chronic arthritis pain and inflammation. It may be a treatment for you and your doctor to consider in managing the painful and continuing symptoms of your medical condition.
What Is Meloxicam?
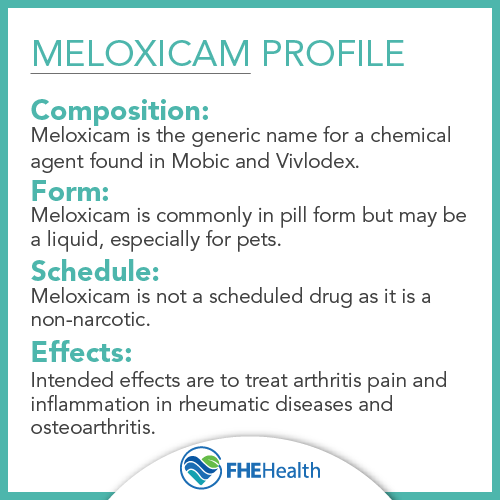
Meloxicam is the generic name for a long-acting, prescription, nonsteroidal anti-inflammatory drug (NSAID). Mobic, approved by the Food and Drug Administration (FDA) in April 2000 for the treatment of inflammation and pain stemming from osteoarthritis and rheumatoid arthritis in adults, is the meloxicam brand name. Meloxicam is also FDA-approved to treat children over the age of 2 who are diagnosed with juvenile arthritis. The drug is marketed by Boehringer Ingelheim Pharmaceuticals, Inc..
What Is Meloxicam Used For?
Meloxicam is prescribed for the treatment of inflammation and pain from osteoarthritis and rheumatoid arthritis in adults and juvenile arthritis (but not for children under the age of 2). The drug is also effective in treating gout pain and inflammation and, according to MedlinePlus, may be used to treat ankylosing spondylitis (arthritis affecting the spine). While meloxicam may be used off-label for other conditions, it’s best prescribed for indications that have clinically proven effectiveness with the NSAID drug.
The pain medication shouldn’t be used by anyone who’s allergic to the drug or who’s had a previous attack of asthma or severe allergic reaction from aspirin or another NSAID. Women who are pregnant or trying to become pregnant should not take meloxicam during the final 3 months of pregnancy because the drug may be harmful to the unborn infant.
How Does Meloxicam Work?
Meloxicam helps reduce hormones in the body that cause pain and inflammation. Available in oral tablet, capsule and suspension forms, meloxicam is usually given as a smaller initial dose, with a higher maintenance dose for those requiring greater analgesic relief. Adult oral dosage strengths include 5-milligram, 7.5-milligram, 10-milligram, and 15-milligram tablets in 7.5 milligrams/5 milliliter suspension. Pediatric oral suspension doses are significantly lower per day, usually 0.125 milligrams once daily, with a maximum of 7.5 milligrams once per day. Meloxicam should be taken at the same time daily and may be taken with or without food. However, taking it with food reduces potential gastrointestinal upset.
What Are the Side Effects of Meloxicam?
Side effects of meloxicam include anemia, abdominal pain, edema and insomnia. If you experience the following less common side effects, you should contact your doctor immediately:
- Allergic reaction symptoms, including hives or welts, itching, skin discoloration or redness and swelling of the eyelids, face, throat, tongue, lips, hands, legs or feet
- Bloating and gas
- Diarrhea
- Headache
- Heartburn or indigestion
- High or increased blood pressure
Other side effects, considered rare, include:
- Body heat loss
- Persistent or hoarse cough
- Fever with or without accompanying chills
- Foul breath
- Lightheadedness, fast or weak pulse or tightness in the chest
- Pain in the muscles or joints or severe stomach pain
- Skin problems, such as clammy or cold skin, skin that blisters, loosens or peels, rash in an area, cracked, scaly skin, skin lesions (including a purple center) and swollen skin that’s also red
- Stools that are clay-colored or appear black, tarry or bloody
- Swallowing difficulty
- Tiredness or weakness that’s unusual
- Urination difficulties, such as significantly decreased frequency of urination and/or amount of urine
- Ongoing vomiting or vomit containing blood or material the consistency of coffee grounds
Severe Risks of Taking Meloxicam
In addition, there are a host of side effects that are uncommon or rare, such as abnormal dreams, nervousness and anxiety, changes in vision, tinnitus, feelings of discouragement or loss of interest or pleasure in doing things once enjoyable, thinning hair, sunken eyes and wrinkled skin.
Severe risks associated with taking meloxicam include FDA-boxed warnings for the following:
- Meloxicam use poses an increased risk of cardiovascular events, such as heart attack, heart failure, blood clots and stroke, any of which may prove fatal. Notably, these risks, which may occur early during treatment, may also increase with ongoing use. Therefore, if you’re prescribed meloxicam, your doctor will need to monitor your blood pressure throughout your treatment regimen.
- Use of NSAIDs, such as meloxicam, may increase the risk of gastrointestinal (GI) events and disturbances, including stomach or intestinal perforation, gastric bleeding and stomach ulcers, which may result in death. Such adverse events may occur without warning and at any time during meloxicam treatment. Adults, especially older adults, with prior incidents of gastrointestinal disease or peptic ulcers are at greater risk for gastrointestinal events. As a result of this severe risk, your doctor will need to actively monitor you for any signs of GI bleeding.
Meloxicam and Kidney Function
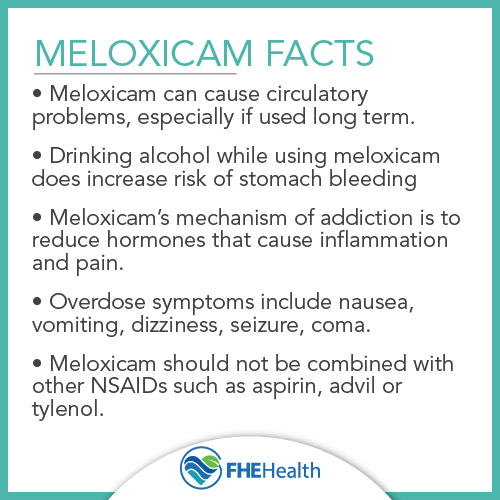
One possible side effect of long-term meloxicam use is kidney damage. Like most NSAIDs, meloxicam limits blood flow to the kidneys by narrowing the blood vessels. Individuals who have a history of kidney disease or those who take additional drugs that harm the kidneys, such as laxatives, ACE inhibitors and antacids, may be at a greater risk of effects. Any changes in urination while on the medication may be a sign of kidney issues.
Meloxicam and Heart Disease
Individuals with heart disease should avoid the use of meloxicam and other NSAIDs unless under the care of their physician. Because NSAIDs impair the ability of the kidneys to remove fluids, this can overwhelm the heart and its ability to pump blood effectively. If you experience chest pain, chest discomfort or weakness on one side of the body while taking meloxicam, call 911 or have someone take you to the emergency room immediately.
How Long Does Meloxicam Stay In Your System?
According to the FDA’s label for Mobic, meloxicam has a half-life of between 15 and 20 hours. At this rate, it will take about 80 hours for the drug to be completely removed from your system, mostly excreted in the form of metabolites in equal amounts through urine and feces. Meloxicam can be detected in your blood for up to 5 days.
Is Meloxicam Safer Than Opioids?
Meloxicam is a safer option in managing mild to moderate pain than opioids. Close to 4% of adults in the United States abuse opioids each year due to the high risk of addiction. Also referred to as narcotics, opioids come with side effects that include slowed breathing, liver and kidney problems, dry mouth, severe itching and depression, even when taken at the lowest dose. Opioids are meant for short-term use and should be taken as prescribed.
Is Meloxicam Addictive?
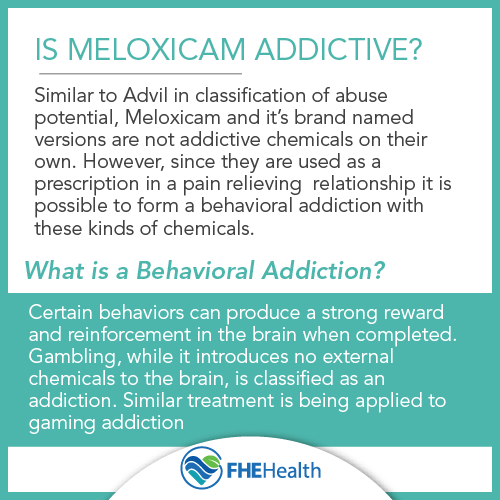
Because meloxicam is an NSAID and not a narcotic medication, and it has no addictive properties, you can’t become addicted to the chemicals in meloxicam. This doesn’t mean, however, that there aren’t potential short- and long-term dangers if you abuse this drug. Any drug, including ibuprofen, another NSAID, can be abused as an element of a process addiction behavior.
Signs of Short-Term Meloxicam Abuse
Signs that indicate short-term abuse, meaning you’re taking the drug more often than prescribed and/or combining meloxicam with alcohol, other prescription drugs or other NSAIDs, include:
- Taking more of the drug in an effort to achieve maximum pain relief. Those who do so may believe (in error) that because meloxicam reduces inflammation and pain, taking more of the drug can achieve relief quicker and last longer. Signs include running out of prescriptions earlier than expected, doctor shopping to secure new prescriptions, stealing someone else’s pills and engaging in secretive behavior using the medication.
- Drug interactions, which may be mild, moderate or serious, can result from taking meloxicam with more than 300 different medications. Major drug interactions may occur with Warfarin or other blood thinners, while moderate drug interactions may occur when taking meloxicam and Cymbalta, Lexapro, metoprolol, prednisone and Zoloft, to name a few.
- Using meloxicam as a recreational drug in a vain attempt to achieve a high. This is illogical because meloxicam is an NSAID and has no addictive properties.
- Combining meloxicam with alcohol and other drugs. This can happen accidentally or in an effort to achieve a euphoric effect (a sign of drug abuse in the latter case).
Signs of Long-Term Meloxicam Abuse
Signs of long-term meloxicam abuse include:
- Overdose, with symptoms that include coma, difficulty breathing, extreme drowsiness, bloody vomiting, bloody stools and seizure
- New or worsening liver or kidney problems
- Co-occurring alcohol addiction and/or addiction to other prescription or illicit drugs
- Sudden heart attack
The Potential for Misuse
Meloxicam isn’t habit-forming, but misuse is possible when not taken as prescribed. Drinking alcohol while taking meloxicam increases an individual’s risk of stomach bleeding. Additionally, those who exceed the prescribed dosage in an attempt to alleviate pain may notice an increase in severe side effects. Older adults may experience an increase in symptoms, and it’s important to speak with a physician before taking any other medication, as deadly side effects can occur.
What are the Treatment Options for Meloxicam?
While you don’t need medical detox to come off meloxicam, you may need to transition from this NSAID drug to one that’s weaker or available as an over-the-counter treatment for pain and inflammation. Psychiatric counseling may also make your transition from meloxicam to another drug or alternative treatment method easier and address any long-term damage you’ve experienced as a result of lengthy meloxicam use.
While you transition from meloxicam use, you may experience a few unpleasant but harmless symptoms. These aren’t like withdrawal symptoms that occur when discontinuing a narcotic medication, but they may be a bit disconcerting at first. Be aware that you could encounter:
- Some jitteriness
- Anxiety over pain coming back
If your pain and inflammation do come back, you should ask your doctor for another effective prescription medication for your osteoarthritis or rheumatoid arthritis that’s nonaddictive and safe to change over to. It’s possible that Celebrex, a selective COX-2 inhibitor and an NSAID medication that’s similar to meloxicam but with fewer gastrointestinal side effects, may be a viable alternative.
You don’t have to suffer while trying to cope with the pain and inflammation caused by your medical condition. Help is available to address any concerns you may have over behavioral dependence on NSAIDs like meloxicam and co-occurring alcohol or other drug use.
Meloxicam is highly effective for treating mild to moderate pain. Discover the side effects and the potential for misuse or addiction when using meloxicam.
Is Meloxicam Addictive?
What Are Treatment Options for Meloxicam?
If you or someone you love struggles with addiction to pain medications, we can help. Contact us at FHE Health to speak to one of our counselors and get answers to any questions you may have about recovery.