
|
|
It’s 2017, Chicago, and Chris Rogers is walking the three blocks from his parking spot to the front door of his apartment building. He passes a park and sees a woman motionless on the ground. He approaches her and recognizes it immediately — an overdose.
He has to make the split-second decision between administering CPR or calling for help. There’s a woman sitting on a park bench 50 yards away who hasn’t noticed the incident.
Rogers yells for help and turns back to the victim. Luckily, the neighborhood’s fire station is directly on the other side of the park. The woman, Tanya Harris, sprints to the station and calls for help.
Two firefighters come running over with their supplies. One of them carries a small pack, which he rips open to reveal a white plunger.
He puts the plunger under the victim’s nose and pushes. The victim regains her breathing, and after an assessment by EMS first responders, her vitals are closer to normal.
According to Rogers, the fact that the victim survived was pure, dumb luck. Before the incident, he didn’t know how to react to what he learned later was a heroin overdose.
The substance administered by the firefighter, he learned, was Narcan, a form of the drug naloxone in a nasal spray. Now, says Rogers, he never leaves home without the drug in his bag, for fear that this could happen again.t
What Is Narcan?
 Opiates like heroin, fentanyl, morphine and prescription opioids bind to receptors and depress the pulse and the respiratory system. In an overdose, both systems begin to shut down, and if nothing is done, an overdose can be fatal.
Opiates like heroin, fentanyl, morphine and prescription opioids bind to receptors and depress the pulse and the respiratory system. In an overdose, both systems begin to shut down, and if nothing is done, an overdose can be fatal.
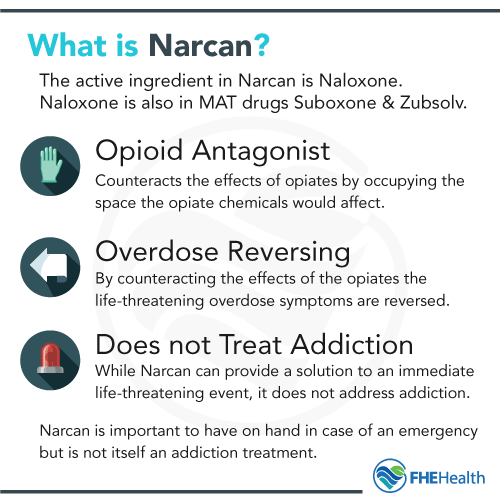
Naloxone is an opioid antagonist, which fights for space in the brain with the opiates. This causes it to reverse the effects of the drug, reversing the overdose in the process.
Narcan has been described as a miracle drug because it effectively brings a person dying of an overdose back to life. That’s why it’s absolutely essential if a family member or other loved one is experiencing the disease of addiction.
Who Uses Narcan?
Naloxone, the active ingredient of Narcan, is used in addiction treatment in recovery drugs like Suboxone and Zubsolv, in conjunction with a mild opioid called buprenorphine. This has become the gold standard in addiction treatment, replacing methadone.
Because of Narcan’s life-saving potential, it’s carried by law enforcement, firefighters, EMS and hospital employees for quick intervention when literally every second matters. But despite Narcan training programs being more common across the country, most police officers don’t carry the substance with them at all times.
Limitations of Narcan
With all of the good that Narcan can do for someone experiencing an overdose, the downsides of the substance get overshadowed. There are very few people who can honestly argue that the drug, in a vacuum, isn’t good for society, but it’s a mistake to proclaim it as the fix for addiction. Here’s why.
First, Narcan, like most drugs, isn’t 100% effective. Many users need a second dose to continue suppression of opiates within a few hours of the first. For this reason and others, a Harvard study of over 12,000 administrations of naloxone in a hospital setting showed that over 6% of overdose victims would not survive the trip to the ER.
Plus, the status quo doesn’t involve any follow-up after Narcan is used, and it’s effects are only temporary. The same study found that 10% more of the patients studied died within one year. This means that while Narcan is miraculous in the short term, it doesn’t do much to help recovery.
Another limitation is that even when bystanders have access to Narcan, it can be misused because people who haven’t had training don’t know how or when to give Narcan. This doesn’t mean that people shouldn’t carry Narcan, just that it takes more than possession of the drug for it to be a life-saving tool.
Does Carrying Narcan Mean You Don’t Trust Your Loved One?
 This a common question people ask when considering acquiring Narcan: If I get Narcan in case a loved one overdoses, doesn’t that show that I don’t trust them?
This a common question people ask when considering acquiring Narcan: If I get Narcan in case a loved one overdoses, doesn’t that show that I don’t trust them?
Not at all. Many addicts owe their lives to a loved one with Narcan in their possession.
Addiction is a chronic, relapsing disease. NIDA reports that the relapse rate for addiction is on par with conditions like asthma, diabetes and hypertension.
It’s akin to a diabetic person having high blood sugar and not carrying their insulin with them. If there’s a life-saving tool with the potential to help you in case of an emergency, wouldn’t you want to have it?
Even if your family member or loved one would be offended, sometimes carrying naloxone without their knowledge, just in case, can be a white lie. They may be upset if they knew, but the alternative could be much worse. The drug may not even be used to save their life, but one of their friends. With the high relapse rate of early recovery, it’s practical to make sure the drug is available in groups of friends in recovery.
To learn more about the complex nature of drug use in the family setting, read our blog here.
The Availability of Narcan and Naloxone
So you’ve made it this far, and you want to get access to naloxone for yourself or a loved one. Where do you start?
While the laws surrounding Narcan and where it’s available are different in different states, you can usually get it at a pharmacy counter at your local Walgreens, CVS, Rite Aid or another store.
Some are surprised to find that they don’t need a prescription for Narcan, and in many cases, the drug is covered under health insurance plans.
Who Should Carry Narcan?
EMS, fire crews and police officers should all carry Narcan — and most do. But, who else should have this drug handy at all times?
If you have a loved one or family member suffering from an addiction to opiates, you should definitely ensure that you have easy access to naloxone, as should anyone who works near addicts, in a treatment environment or otherwise.






