SHATTERPROOF FHE Health First Responders’ Program
First responders heroically serve our country every day. By being the first to arrive on the scene in crises, disasters, emergencies, wars, and other violent events, they suffer disproportionately from exposure to trauma and trauma-related stress and its mental health effects.
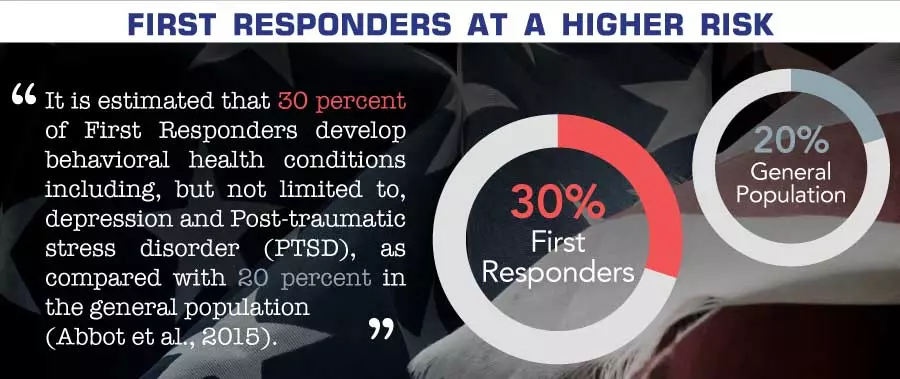
The Substance Abuse and Mental Health Services Administration (SAMHSA) has reported that roughly one in three (30 percent) of first responders—that is, police officers, firefighters, and emergency medical services (EMS) personnel—develop a behavioral health condition as a direct result of their work. The real number, accounting for those who are slow to report problems or live with undiagnosed symptoms, is inevitably much higher.
Trauma-Related Symptoms
Because trauma is a common occupational hazard in their profession, first responders are more at risk of trauma-related mental health issues like PTSD and depression. Some of the symptoms they might experience include:
- emotional numbness
- avoidance of people, places, or things that are reminders of the event
- a loss of pleasure in things that once brought joy
- high reactivity to certain situations
- sleep problems
- problems with drugs, alcohol, or food
These and other symptoms are often very treatable, yet many first responders suffer in silence, out of fear they could lose their job or be labelled as weak or unfit to serve. Many also worry they may be the only one struggling among their peers.
What Is Specialized Treatment for First Responders?

A specialized treatment program such as Shatterproof at FHE Health:
- addresses the unique stressors, triggers, and experiences that first responders face;
- aligns with first responders’ culture, code, and values;
- helps first responders recover as quickly as possible, so they can return to their families and to service in their communities.
Shatterproof FHE Health (formerly Florida House Shatterproof) employs evidence-based therapies, innovative medical care, and a comprehensive wellness program to help first responders successfully manage their condition and/or achieve life-long recovery from drugs and alcohol. We take a holistic treatment approach that attends to the physical, neurological, mental, social, emotional, and spiritual aspects of wellbeing. Our medical and clinical team creates a customized, individualized plan of care to help our first responders:
- address the underlying issues contributing to symptoms
- face and overcome specific obstacles
- increase their ability to manage emotions in stressful situations
What Are the Unique Features of Shatterproof FHE Health?
 First responders in our program regularly attribute their success in treatment to these three unique components of Shatterproof FHE Health:
First responders in our program regularly attribute their success in treatment to these three unique components of Shatterproof FHE Health:
- Intensive EMDR Program
- Neuroscience-Based Treatments
- A Peer Community of First Responders
Intensive EMDR Program
This is a new, comprehensive program to bring intensive EMDR therapy to our patients, many of whom have had significant exposure to trauma and have experienced profound benefits from EMDR. “Eye Movement Desensitization Reprocessing” is a highly effective, neuroscience-and-evidence-based trauma therapy. More than 30 years of research supports its use. A gold standard in trauma treatment, EMDR has relieved symptoms for many people, by desensitizing, reprocessing, and reconsolidating traumatic memories.
Intensive EMDR accelerates this therapeutic work, allowing many of our patients to experience symptom relief and memory reconsolidation much more quickly and comprehensively. The longer EMDR sessions are designed to build tolerance for and achieve resolution from trauma-related symptoms. When not engaged in memory reprocessing, the patient takes breaks by using skills with resourcing from the EMDR therapist. This program works particularly well for first responders—for a variety of reasons.
Neuroscience-Based Treatments
 FHE Health’s innovation in using the latest brain technologies to treat PTSD and other mental health conditions is rare among behavioral health providers nationwide. Shatterproof FHE Health patients are able to make use of these neuroscience-based treatments in conjunction with other therapies. The result is a speedier recovery, so that patients can return to their families and communities as soon as possible.
FHE Health’s innovation in using the latest brain technologies to treat PTSD and other mental health conditions is rare among behavioral health providers nationwide. Shatterproof FHE Health patients are able to make use of these neuroscience-based treatments in conjunction with other therapies. The result is a speedier recovery, so that patients can return to their families and communities as soon as possible.
After their admission to our facility, each patient receives a neuroimaging scan of their brain that identifies areas of dysfunction related to PTSD and other mental health symptoms. When patients are able to see empirical evidence of their illness on a scan, many of them are able to let go of their shame and self-stigmatization: They are able to see and accept that they have a verifiable medical condition. Meanwhile, the brain imaging scans allow us to then therapeutically target impaired areas of the brain with cutting-edge technologies that relieve PTSD symptoms and restore brain health.

A Peer Community of Other First Responders
Research has uncovered the importance of belonging for first responders who seek rehab. For example, a study at the University of Buffalo found that veterans have better healthcare outcomes when their providers are familiar with military culture and values. From our own experience, too, when first responders can be part of a supportive community of peers, they feel more comfortable sharing and processing their experiences. They are more apt to participate in group therapy, because they know that the others in the room can truly understand what they are going through. This healing power of peer community has improved outcomes for our first responders.

What Are Shatterproof FHE Health‘s Levels of Care?
 First responders in Shatterproof FHE Health can receive a continuum of care consisting of these three levels of care, as defined by the American Society of Addiction Medicine (ASAM):
First responders in Shatterproof FHE Health can receive a continuum of care consisting of these three levels of care, as defined by the American Society of Addiction Medicine (ASAM):
- Level 1: Outpatient Services do not require that a patient live on-site at our facility, although designated housing for first responders is provided. It permits patients to attend to work and home responsibilities while engaging in group and individual therapies. (Ex: The firefighter above who develops depression might best be served by this option in the earlier stages of his depression.)
- Level 2: Intensive Outpatient (IOP) or Partial Hospitalization (PHP) entails significantly more time in group and individual therapies and treatment than do outpatient services, but without the residential requirement.
- Level 3: Residential/Inpatient Services are the highest, most intensive level of care for first responders with more severe and co-occurring mental health conditions. Patients are in supervised care 24/7 while receiving a full, intensive day of group and individual therapies. (Ex: The firefighter who waits to get help until he has co-occurring depression and alcoholism will be better served at this level of care.)
Following a program of treatment at one of the above levels of care, graduates of the program can enjoy the many benefits of our Alumni and Aftercare Program, including:
- Our strong alumni support system
- Group meetings like those in Alcoholics Anonymous and Narcotics Anonymous
- Individual therapy sessions
Stigma and Other Perceived Barriers to Treatment Among First Responders
Mental health issues are common conditions in the U.S. and globally. They are also treatable much of the time but can become serious and even life-threatening in the absence of medical treatment.
Even so, the stigma surrounding mental illness can prevent people from seeking help. This stigma can be an even bigger deterrent within a first responder culture that celebrates being “tough” and “heroic” in the face of emergencies.
Limited insurance coverage is another perceived barrier to treatment. Worries that an existing medical insurance plan won’t cover mental healthcare needs are not unusual. The expense associated with routinely seeing a therapist and/or psychiatrist may also cause stress.
The good news is that mental health care is medical healthcare and that insurers include mental health coverage in their plans today. Also, many employers and first responder unions are aware of how crucial mental and emotional wellness is to employee performance and productivity—and, that many mental health symptoms can be successfully managed with treatment.
Employees who proactively seek treatment and manage their condition before it could worsen demonstrate a healthy response to a medical issue. If you are a first responder and have concerns about treatment, talk to your doctor. Ask for more information and guidance, so you can make the right decision for your needs.
Job-Protected Treatment – Another Benefit of Shatterproof FHE Health
 As dedicated public servants with a strong ethic of self-sacrifice, first responders are often the last to ask for help for themselves. They also have concerns that seeking treatment for a mental health issue could endanger their job.
As dedicated public servants with a strong ethic of self-sacrifice, first responders are often the last to ask for help for themselves. They also have concerns that seeking treatment for a mental health issue could endanger their job.
At FHE Health, we have created an admissions process that is discreet and confidential, with the guarantee that your employer won’t have to find out. Our in-house expertise allows us to work closely with first responder unions to protect your job, so you can focus on your recovery with peace of mind.
How Help for You Is Heroic
Showing up for other Americans in their time of need and crisis, even if it means putting one’s own life at risk, is honorable and heroic. But only a superhero can constantly stand in the line of fire without being affected.
If you’re struggling with a mental health problem, do the honorable and heroic thing today and show up for yourself, by calling us today. We’re here to help you the rest of the way.